Sex After Vaginal Atrophy Is Possible
Aging is a natural part of life, but no one told us that our aging vagina would impact our sex lives. As if the hot flashes, mood swings and bodily changes weren't enough, now we can add painful intercourse, vaginal dryness and a loosening labia to the mix. Vaginal atrophy is a painful condition that many of us are embarrassed to talk about, but breaking through this barrier can help you return to a healthy sex life.
How do I know if I have vaginal atrophy?
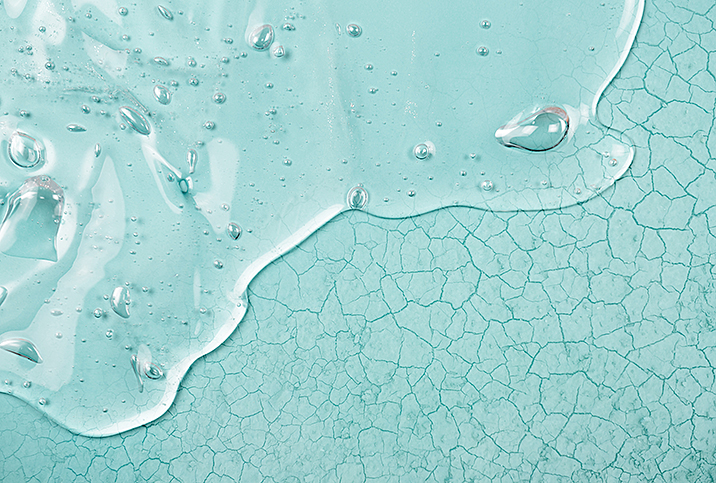
Vaginal atrophy, or atrophic vaginitis, is a common condition that impacts the vagina, the vulva and the urinary tract. This condition can cause pain during sex, vaginal dryness, bladder weakness and incontinence, and can impact the appearance and elasticity of the vulva.
Typically, this condition is most common as we approach menopause. However, it also affects women during any health event that impacts estrogen levels, such as cancer treatments, reproductive surgery or when taking hormone treatments related to endometriosis or even certain birth control pills.
Diagnosing vaginal atrophy is a multistep process that includes discussion of symptoms, a pelvic exam and a urinalysis for pH balance. In rare instances, your doctor may also order lab work to check your hormone levels. Once your doctor has all the information, an appropriate treatment plan can be created. The most important aspect of this process is your openness in discussing your symptoms.
Managing your symptoms can take time, but eventually you will find a treatment plan that can allow you to return to the sex life you want.
It's essential to provide all your symptoms and complications, because while vaginal atrophy is common, other more serious conditions, such as cervical cancer and endometriosis, can cause similar pain. The more precise you are in describing your symptoms, the easier it will be to diagnose your condition.
Medicinal treatments
As vaginal atrophy is caused by changes in estrogen levels, increasing the local estrogen levels within the vaginal tissue using vaginal creams, rings or pills can restore elasticity and increase lubrication.
Unfortunately, using hormonal treatments can come with its own risks. An increase in estrogen can intensify the symptoms of reproductive complications, such as endometriosis and polycystic ovarian syndrome (PCOS). Hormonal treatments are also not recommended for women undergoing cancer treatment or recovering from cancer treatment because an increase in estrogen may trigger cancer regrowth.
The specific treatment your doctor prescribes will be based on your personal and familial gynecological history. And if you had cancer, consult with your oncologist before receiving hormone treatments.
Natural alternatives
Most healthcare providers recommend nonhormonal treatments as a first step in overcoming your symptoms to avoid any unexpected complications. This is an important step in your treatment plan because trying these natural treatments can eliminate the lesser symptoms and help to pinpoint the most impactful complications of your condition without altering your body chemistry.
Most often, purchasing an over-the-counter (OTC) vaginal moisturizer and applying it daily and using a long-lasting, glycerin-free vaginal lubricant is enough to overcome this chronic condition.
If you try these topical treatments and your symptoms continue or remain unchanged by these interventions, your doctor may recommend vaginal dilators and pelvic floor exercises to strengthen and improve the elasticity of the vaginal walls.
These treatments are also accessible without a prescription, but they provide a more intensive treatment, which can include physical therapy to strengthen the pelvic muscles in addition to the pelvic floor. This treatment is especially helpful in addressing bladder weakness and incontinence.
Managing your symptoms
Finally, if all these treatments fail to fully address your symptoms, your doctor may prescribe a hormone-free medication that can alleviate painful intercourse. This can include a vaginal numbing agent or daily pill. However, many doctors like to avoid these treatments as they numb the vaginal tissue, which can make you more susceptible to vaginal tears and other injuries.
Managing your symptoms can take time, but eventually you will find a treatment plan that can allow you to return to the sex life you want. Documenting your symptoms leading up to diagnosis and continuing to monitor these symptoms as you undergo treatment is essential in helping your doctor accurately manage your vaginal atrophy.