How Can You Prepare for Surgical Menopause?

All of a sudden, everyone is talking about menopause. At least, that's how it seems.
Menopause talk is prevalent, with Oprah discussing her experience of being brushed off by doctors in perimenopause and actress Naomi Watts launching her new line of "menopause solutions."
Yet, surgical menopause—menopause caused by the removal of ovaries—isn't usually in the conversation. In fact, I'd never heard the term—until I found myself facing the surgery myself.
So what is it, why would it be needed and how can you prepare for surgical menopause?
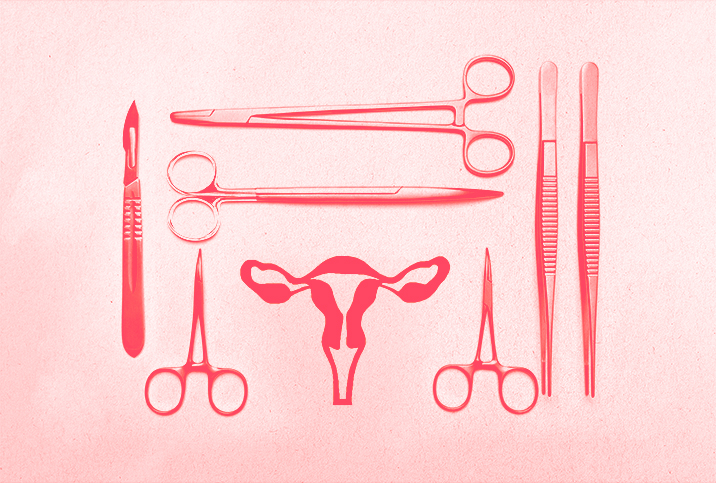
What is surgical menopause?
Surgical menopause is menopause caused by the removal of both ovaries—also known as a bilateral oophorectomy—and can happen before the normal age of menopause.
Menopause is a natural biological process that happens to women in their 40s or 50s. It is diagnosed after 12 months without a menstrual period. According to Mayo Clinic, the average age for menopause is 51 for American women.
"The most urgent reason to remove both ovaries is if the patient has or is at high risk of developing ovarian cancer," said Nisarg Patel, M.B.B.S., M.S., the director of the Nisha IVF Centre in Ahmedabad, India.
A bilateral oophorectomy may mitigate painful conditions such as ovarian cysts, tumors or abscesses, he added. In the case of unilateral oophorectomy, in which only one ovary is removed, ovarian function is preserved and the patient does not go through surgical menopause.
What events lead to surgical menopause for some women?
While in labor with my third child, my uterus ruptured. What ensued was an emergency C-section, followed by an emergency hysterectomy and bilateral oophorectomy.
I emerged from the hospital with my life and my daughter's life intact but with little understanding of where I suddenly found myself. In menopause. I hadn't expected to arrive in that territory for at least another 15 years.
Fortunately, most patients facing surgical menopause have more opportunities to prepare for their body's coming hormonal upheaval. They have time to incorporate the dietary changes and hormone therapies that can help women through this transition.
How can you prepare for surgical menopause?
"Women who undergo surgical menopause before natural menopause occurs can face a harsher entry into menopause due to the abrupt cessation of ovarian function," Patel said.
The removal of the ovaries stops the production of estrogen and progesterone, which can cause the sudden onset of menopause symptoms.
These menopausal symptoms may include the following:
- Hot flashes
- Insomnia
- Loss of libido
- Mood swings
- Night sweats
- Vaginal dryness
Low estrogen levels can put women at an increased risk of multiple adverse long-term health effects, such as complications with cardiovascular health, osteoporosis and cognitive decline.
"Women may want to consider taking hormone replacement therapy (HRT) as prescribed by their doctor," Patel said. Estrogen can help reduce the symptoms of menopause.
Women who have not undergone a hysterectomy in addition to an oophorectomy—in other words, women who haven't experienced the removal of a uterus—should take progesterone combined with estrogen. Why? Estrogen without progesterone may increase uterine cancer risk, according to the American Cancer Society (ACS).
Women preparing for surgical menopause should consult with their doctor about which HRT treatment options may be right for them.
"Some women may have contraindications or preferences that make HRT unsuitable for them," Patel said.
These groups include women with a history of breast cancer, blood clots or stroke who may not be able to take HRT safely.
What can you do to maintain your physical health after bilateral oophorectomy?
The decline of estrogen in menopause can slow down metabolic function and could cause a decrease in bone density and a loss of muscle mass. In addition to HRT, a healthy diet may improve the negative effects of menopause.
Women in surgical menopause may experience more energy and increased quality of life via a menopause-supportive diet. A low-fat, plant-based diet—the Mediterranean diet is one possibility—can improve a woman's health, according to a 2021 study.
Iron-rich foods such as lean red meat, poultry, leafy green vegetables and nuts are excellent sources of protein and can help to maintain muscle mass that can decline in menopause. It's also important for menopausal women to drink plenty of water and get enough fiber.
What can you do to maintain your mental well-being after bilateral oophorectomy?
"Women should consider the emotional element of undergoing bilateral oophorectomy and entering surgical menopause," said Shara Cohen, Ph.D., a research scientist and the founder of Cancer Care Parcel in Barnet, England. "Psychological and emotional support is vital for bilateral oophorectomy patients to help patients deal with the onset of menopause symptoms and feelings that may arise from the sudden loss of fertility."
With a full picture of the patient's HRT needs and psychological state, physicians can tailor support to each individual. Women experiencing surgically induced menopause have different needs and concerns. There is no one-size-fits-all standard of care.
Why is HRT important for women with surgical menopause?
Life expectancy after oophorectomy, particularly in women who experienced bilateral oophorectomy before age 47 and a half, remained consistent with women who kept their ovaries. If the women began HRT with estrogen, that is, a 2014 study suggested.
Women who did not begin HRT after oophorectomy experienced a marked rise in mortality, leading to a 41 percent increase in all-cause morbidity from cancer, stroke, congenital heart defects and cardiovascular disease.
Given the potential negative long-term effects of bilateral oophorectomy—particularly before the natural onset of menopause—it's essential that women considering the procedure for any reason speak with their healthcare providers, understand the risks and learn how to manage them.
Should I be scared of surgical menopause?
If you're looking for horror stories about surgical menopause, the internet is full of them. (Don't look.) But facing surgical menopause doesn't have to be nightmare-inducing.
When I entered surgical menopause, my husband and I knew our family was complete. My OB-GYN started me on an estrogen patch in the hospital. My one dreadful menopause symptom has been—brace yourself—dry hands every now and then. I definitely haven't missed having my monthly period.
All in all, it's not so bad. I'd even say surgical menopause (for me) is better than OK. If you're facing surgical menopause, take heart. With the right tools and a healthy support system, there is life after ovaries.