Ovarian Cancer: Myths & Misconceptions
In America every year, about 22,000 new cases of ovarian cancer are diagnosed, and more than 14,000 fatalities are attributed to the disease, making it the fifth-deadliest cancer for women. Given that status, however, ovarian cancer is rarely detected through routine checkups.
Personal awareness of this disease is essential. Know the facts that debunk the myths, and make sure you discuss any unfamiliar symptoms with your doctor.
Myth: The HPV vaccine helps prevent ovarian cancer.
Reality: The HPV vaccine can prevent most types of cervical cancer if it is administered before a girl or a boy is exposed to the human papillomavirus (HPV). It does not, however, prevent ovarian cancer. Incidentally, the HPV vaccine also helps to reduce the risk of vaginal, vulvar and anal cancers, and the medical conditions associated with them, since those cancers can be caused by HPV. There is no association between HPV and ovarian cancer.
Myth: There is a solid set of symptoms to watch out for.
Reality: Ovarian cancer symptoms are not easily detected. The symptoms may feel like normal sensations, including stomach bloating or normal period cramps. Symptoms such as persistent heartburn, unusual pain during intercourse, a more frequent need to urinate, backaches, irregular cycles, bleeding between periods and even recurring constipation are good reasons for any woman to seek medical attention immediately. Ovarian cancer symptoms are not easy to analyze without proper cancer screening procedures, and invasive surgery may be required for a thorough diagnosis.
Myth: A Pap smear or other tests can detect ovarian cancer.
Reality: A Pap smear is a cancer screening procedure used to detect cervical cancer only; it does not help determine whether you have ovarian cancer. Since a Pap smear is usually administered during their annual OB-GYN health exam, many women believe they are covered by the Pap smear for other cancer detection. They are not, but the belief creates a false sense of security when the test comes back as normal.
The CA 125 test is administered to test the blood for changes in the cancer antigen 125 protein, and to monitor patients during and after treatment for cancer. The CA 125 test produces too many false positives and false negatives to be solely relied upon as a screening test for ovarian cancer, although this test is sometimes used as an indicator for women who are at extremely high risk for ovarian cancer. CA 125 is elevated in epithelial ovarian cancers, but other benign gynecological conditions, such as ovarian cysts, fibroids and endometriosis, and non-gynecological conditions, like gallbladder disease, can cause an elevation in CA 125. Therefore, the test is not ordered for everybody.
At this point, there is no screening tool for ovarian cancer.
Myth: An annual checkup with my OB-GYN will catch ovarian cancer.
Reality: Because there are no screening tests for ovarian cancer, it is unlikely that any regular tests or examinations will provide the doctor with any evidence that you might have ovarian cancer. Most important, if you have any symptoms you can’t explain, it is important to discuss those with your doctor, as well as any risk factors and family history of cancer. Your OB-GYN will probably perform a pelvic exam, as well as various blood tests, such as the CA 125. Further testing could include an ultrasound to check for any suspicious growths or abnormalities, and a gynecologic oncologist may be consulted to determine whether invasive surgery is required to determine an ovarian cancer diagnosis.
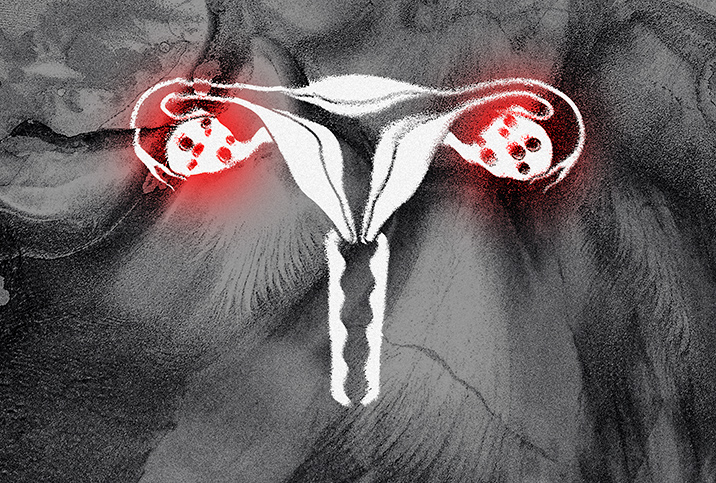
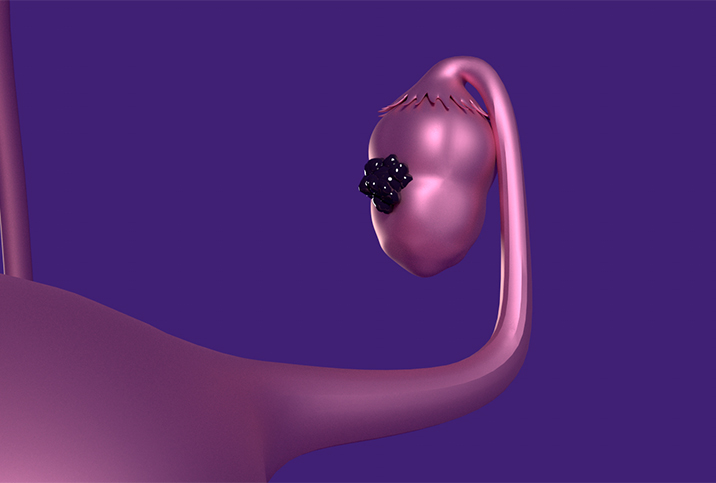
Myth: Ovarian cysts lead to cancer.
Reality: At some point, most women who ovulate have ovarian cysts. Small sacs filled with fluid, ovarian cysts usually develop on or inside the ovaries, but they are no cause for immediate alarm. They are common and often disappear within a few months without the woman needing to undergo any form of treatment.
The U.S. Department of Health and Human Services reports that between 5 and 10 percent of women require an ovarian cyst to be surgically removed, and of those cysts, 13 to 21 percent are malignant. Large or enlarging ovarian cysts usually cause pain and are removed. Complex cysts, which are cysts filled with debris or divisions in the cyst, can be malignant. Simple cysts are benign.
Myth: Using talcum powder can lead to ovarian cancer.
Reality: Recent lawsuits have linked the use of talcum powder to ovarian cancer, resulting in large financial settlements with the companies that use talc in their personal care products. However, this remains a controversial issue. A report published in the Journal of the American Medical Association (JAMA) in early 2020 did find a slightly greater incidence of ovarian cancer in women who had reported using talcum powder in the past, but the National Institute of Environmental Health Sciences and the National Cancer Institute concluded the link is not statistically significant. The report, based on four studies, looked at a total of more than 250,000 women. The findings did not rule out, however, a “small increase in risk” from using talcum powder.
Myth: Ovarian cancer is incurable.
Reality: Contrary to what most people believe, ovarian cancers are not entirely incurable. The problem, however, according to the American Cancer Society, is that approximately 80 percent of all ovarian cancers in the United States are detected after they have already passed the early stages. Ovarian cancer is treatable when detected early enough, and patients who receive early detection have a 94 percent chance of living beyond five years after being diagnosed. Even women with some specific late-stage ovarian cancers can receive treatment and have a good chance of living a long life.
Early detection plays a key role in survival of ovarian cancer. Because the disease is largely asymptomatic in the early stages, women should consult their physician if they feel anything is wrong with their body.