Other STIs/STDs: Myths & Misconceptions

Sexually transmitted infections (STIs) and sexually transmitted diseases (STDs) affect millions of people in the United States each year. Though they're preventable, and in most cases treatable, STIs and STDs still carry a heavy stigma based on out-of-date information or beliefs that were never true in the first place.
Here we’ll take a look at trichomoniasis, pelvic inflammatory disease (PID), and pubic lice.
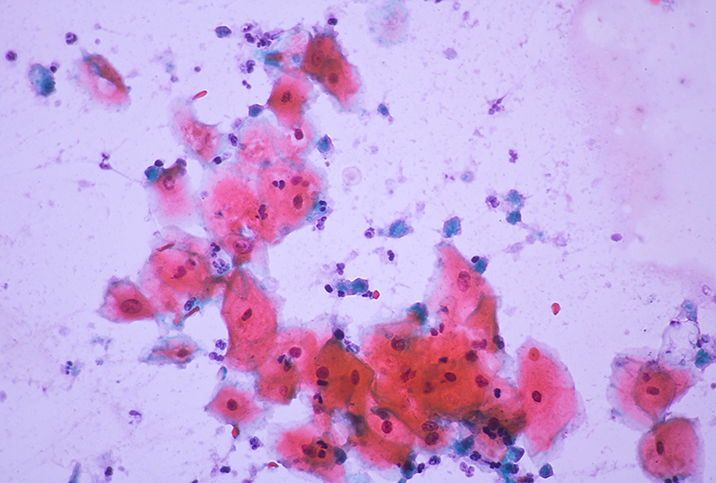
Trichomoniasis
According to the Centers for Disease Control and Prevention (CDC), trichomoniasis is one of the most common STDs, with more than 2 million infections in the U.S. in 2018 alone.
Though trichomoniasis (sometimes called "trich" or "trick") is common—it is spread by a protozoan parasite known as trichomonas vaginalis—many myths still persist about this STD. We tracked down five of the common misconceptions about trichomoniasis and kept digging to find out what the facts actually show.
Myth: Trichomoniasis is easy to detect.
Reality: It's difficult to tell if a person has trichomoniasis because about 70 percent of people infected with trichomoniasis do not develop any visible symptoms, according to the CDC. The only way to find out for sure whether you have trichomoniasis is to get an STD test.
Myth: Trichomoniasis never causes symptoms.
Reality: Because people with trichomoniasis have a reputation for being asymptomatic, many individuals mistakenly believe that this STD never causes symptoms. This isn't the case. Using the CDC information, about 30 percent of infected people feel symptoms, which can include soreness, irritation, pain during urination and penetrative sex, abnormal vaginal or penile discharge, foul smell from the genitals, and the frequent urge to urinate.
Myth: Trich can only be spread through penis-in-vagina sex.
Reality: Usually, the parasite is spread through coitus involving penetration of the penis in the vagina. Still, the parasite can be spread through vagina-to-vagina contact and even through sharing unprotected sex toys with someone who is already infected with this STD. However, it's important to note that medical experts report trichomoniasis cannot be spread through kissing, hugging or by sharing toilet seats.
Myth: There's no cure for trichomoniasis.
Reality: Actually, trichomoniasis is highly treatable. Like most sexually transmitted diseases and infections, trichomoniasis is treated with oral antibiotics, such as metronidazole (Flagyl) or tinidazole (Tindamax), or a vaginal antibiotic cream. If you've been diagnosed with trichomoniasis, you should abstain from sexual activity until you've completed your treatment and tested negative for the condition. And your partner should be treated, too, to prevent reinfection.
Myth: Trichomoniasis isn't dangerous.
Reality: While trichomoniasis is treatable and often doesn't cause any symptoms, it can lead to potentially dangerous complications when left untreated. Women are at a higher risk of difficulties resulting from a trichomoniasis infection. Some potential complications of trichomoniasis include infertility, chronic abdominal or pelvic pain, and scarring of the fallopian tubes. The STD also presents risks to the unborn child of an infected mother. To avoid complications, it's important to seek treatment for trichomoniasis right away.
The only way to prevent trichomoniasis is to abstain from sexual intercourse or to always use protection during sex. Education is critical to slow the spread and keep you healthy. Don't hesitate to reach out to your healthcare provider for more information.
Pelvic Inflammatory Disease
The movement of microorganisms from the cervix to the upper genital tract can result in a clinical syndrome commonly referred to as pelvic inflammatory disease (PID), which causes infection and swelling of the female reproductive organs. In the United States, PID is usually caused by a severe complication of the most infectious sexually transmitted diseases reported: chlamydia and gonorrhea (and other sexually transmitted infections).
Pelvic inflammatory disease is so common in the U.S. that approximately 1 million women are infected annually. Myths and misconceptions surround PID and knowing the most common ones is important. Read on as we debunk them.
Myth: PID is caused only by STDs.
Reality: Even though sexually transmitted diseases (STDs) cause most pelvic inflammatory disease infections, approximately 10 percent of PID infections are transmitted in the absence of STD bacteria.
Non-sexually transmitted PID may happen as a result of:
-
Septic abortions.
-
Use of unconventionally sterilized tools during medical termination of pregnancies.
-
Use of an improperly sterilized curette to remove the endometrium through the cervix.
-
Ruptures in the lower abdominal cavity that lead to the spread of abscesses to the uterus.
-
Other types of bacteria that are not sexually transmitted but can cause PID, such as klebsiella, clostridia, Bacteroides, E. coli, actinomyces, fusobacteria and staphylococcus.
Women can also increase their chances of developing pelvic inflammatory disease in any of the following ways:
-
They engage in unprotected sexual activities (especially for women under the age of 25), have multiple sexual partners or are in a sexual relationship with a partner who has multiple sexual partners.
-
They frequently flush their vagina with water or other fluids, especially douche, which can cause an imbalance of vaginal bacteria.
-
They have a history of STDs and sexually transmitted infections (STIs).
-
They douche, use an intrauterine device (IUD) or use a tampon before the end of the medically recommended healing period after childbirth or abortion. (Six weeks is preferred for pelvic rest after childbirth; two weeks is acceptable following abortion or miscarriage.)
The use of a long-term birth control device inserted in the female reproductive organ, such as an IUD, does not cause pelvic inflammatory disease but can increase the chances of contracting PID when other factors are involved.
Myth: PID is a minor issue.
Reality: Pelvic inflammatory disease is not a minor issue, especially as it most often starts with an STD, which should receive treatment as early as possible. If PID is left untreated for several months, it can quickly spread to other parts of the body and cause chronic pelvic pain as well as complications such as scarring in muscle tissue. It can also destroy the female reproductive organs and cause infertility.
For a woman to detect pelvic inflammatory disease as early as possible, she must know the symptoms of the disease, the most common of which include:
-
A high fever, but without the chills
-
Mild to severe pain in the lower abdomen
-
Bleeding of the uterus during or after intercourse and between menstrual cycles
-
Mild to severe pain during sex and urination
-
Heavy and extremely smelly vaginal discharge
-
Nausea and vomiting
Myth: If I’m still a virgin, I can’t get PID.
Reality: PID can affect all women, no matter their sexual activities. In other words, women who are virgins are still at risk of contracting PID, although it is rare. Most PID cases are due to STDs and STIs, but given that not all cases stem from sexual activity, women need to take precautions such as visiting a doctor for a pelvic exam if they experience pain in their lower abdomen or any other PID symptoms.
Myth: PID is untreatable.
Reality: Pelvic inflammatory disease is treatable if diagnosed early enough, but it can leave irreversible scarring and damage to the fallopian tubes and the whole reproductive system. The earlier this disease can be diagnosed and treatment has begun, the higher your chance of making a recovery. PID may make it difficult for a woman to get pregnant both during and after the ailment period. PID also increases the chance for tubal pregnancies due to the scarring of the tubes. But this doesn’t mean pregnancy is impossible. Some women manage to conceive and deliver healthy babies even after suffering pelvic inflammatory disease. Early detection and early treatment are key.
Pubic Lice
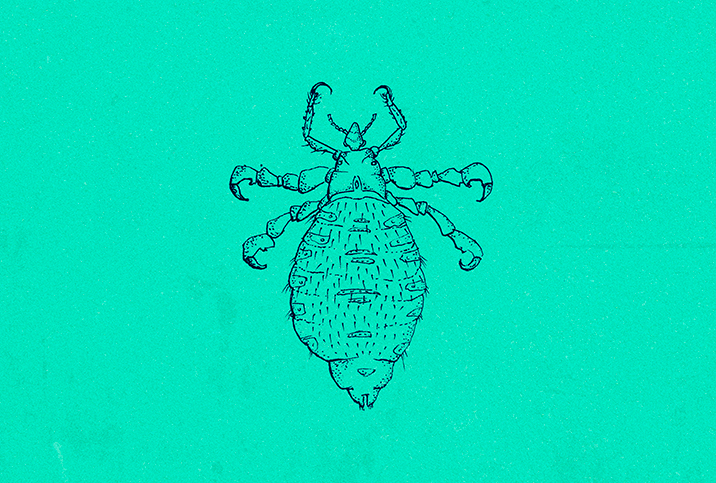
Pubic lice—also known as crabs or crab lice—are tiny insects that inhabit coarse body hair, especially pubic hair, and lay eggs, leading to skin irritation and itching.
Pubic lice are whitish-gray or rust-colored and about a quarter of a centimeter long. They get the name crabs because of their two pincers that help them grip onto hair. Pubic lice affect about 3 million Americans each year, making them quite common, and they're usually spread through sexual activity.
The most noticeable pubic lice symptom is intense itching that starts approximately five days after you get them. The itching is caused by an allergic reaction to the bites. Generally, pubic lice cause discomfort, however, it's possible another bacterial infection could occur due to excessive scratching.
No one wants little crabs in their crotch. Get the facts, stay safe and ditch the itch.
Myth: I can get pubic lice from a toilet seat.
Reality: While not impossible, it's extremely rare to get pubic lice from a toilet seat. Crabs need blood to survive, so they do not live long (typically a day or two) when they're away from a human body. Furthermore, crabs cannot hang on to hard, smooth surfaces like a toilet seat.
Myth: Pubic lice are spread only through sexual activity.
Reality: You can potentially get pubic lice from sharing clothing, towels or bed linens with a person who has pubic lice, though the lice are typically spread by sexual contact. While pubic lice are not a reportable disease—that is, this is not a disease considered to be of great public health importance—they are considered to be a sexually transmitted disease (STD).
Myth: Pubic lice are found only in pubic hair.
Reality: Although crabs are most common in the genital region, they can inhabit other areas of the body, such as leg hair, chest hair, armpit hair, mustache or beard.
Myth: Pubic lice transmit diseases.
Reality: Crabs are not known to transmit any disease, according to the Centers for Disease Control and Prevention (CDC).
Myth: Over-the-counter treatment is the only option.
Reality: If the OTC lotions and mousses don't work, prescription treatments are also available. Lindane shampoo is a common prescription treatment. Because prescription treatments are more toxic, they are not usually recommended by doctors unless other treatments are not working or you can't use an OTC lotion because of an allergy.
You have no reason to be scared of pubic lice. The condition is common, treatable and does not lead to serious health problems. If you have further concerns, speak with your pharmacist, doctor or another medical professional.