Nipple Discharge? Your Doctor May Schedule a Ductogram
Nipple discharge is more common than you may think, and isn't always a sign of something serious. But if the condition is persistent or other symptoms are present (such as pain or a lump), your doctor might recommend a ductogram to figure out what's going on.
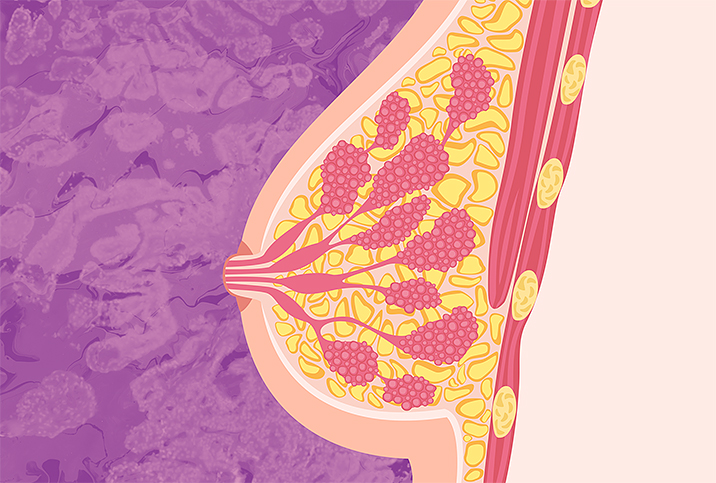
We regret to inform you a ductogram doesn't involve any ducks, which would undoubtedly make the procedure far more interesting than it is. A ductogram, also called a galactogram, is simply a low-dose X-ray examination—very similar to a mammogram—that doctors use when a woman has nipple discharge. What makes it different from a regular mammogram is before the procedure, your breast will be injected with a contrast dye so your doctor can see a more detailed view of the milk ducts. So, you don't get ducks but you do get dye, and that's something, right?
But just what can a doctor tell from a ductogram? And how should you prepare before the procedure? We talked to a few breast imaging experts to find out what you can expect.
What types of discharge warrant a ductogram?
Not all nipple discharges are cause for concern and so not every type will require a ductogram, explained Richard Reitherman, M.D., Ph.D., medical director of breast imaging at MemorialCare Breast Center at Orange Coast Medical Center in Fountain Valley, California.
Nipple discharge can either be "expressible" (it occurs when the breast is squeezed or compressed) or "spontaneous" (it has a seemingly random occurrence), Reitherman said. Spontaneous discharge is more likely to be cancerous, while expressible discharge is probably benign.
If your discharge is bloody or clear and coming from a single duct, your doctor will likely order a ductogram. On the other hand, if your discharge is yellow, gray, green, blue-green or milky, this is less likely to be cause for concern. Doctors aren't as likely to recommend a ductogram when the nipple discharge comes from both breasts.
"Any type of new nipple discharge should be brought to attention, but we are most concerned with unilateral, spontaneous, bloody or clear nipple discharge. This means it's only on one side, comes out on its own (as opposed to being pressed out—some patients notice it on their bra at the end of the day, for example), and the color of red/brown or clear," said Tiffany L. Chan, M.D., an assistant clinical professor for Breast Imaging at the UCLA Department of Radiological Sciences.
A common reason for nipple discharge is an intraductal mass (a tumor growing inside the duct). So, your doctor will primarily be looking for that with the ductogram. If they find a mass, they'll want to make sure it's not cancer or a high-risk lesion. Either way, surgery may be recommended to remove the tumor.
Other reasons your doctor might perform a ductogram
A ductogram may also be performed if your doctor suspects an intraductal papilloma—a wart-like noncancerous lump near your breast. Some papillomas cause discharge, while others do not. If a papilloma is discovered, close observation and/or surgery is generally recommended.
In addition, other abnormal breast conditions that involve the milk ducts, such as fibrocystic changes, ductal ectasia and ductal carcinoma (breast cancer), can be diagnosed using a ductogram.
Images obtained from a ductogram will help direct the surgeon to ducts that require surgical removal for breast cancer and intraductal papillomas.
How to prepare for a ductogram
A ductogram requires very little preparation on your end. However, there are essential things you should and should not do to ensure a successful procedure.
Do's:
- Wear comfortable clothing you can easily remove from the waist up.
- Tell your doctor about any allergies and past illnesses.
- Be forthcoming with your doctor if you are possibly pregnant.
Don'ts:
- Ductograms are most successful when you can elicit a single duct nipple discharge. Therefore, do not squeeze your nipple before the test.
- As with an X-ray examination, the basic rule is to remove any interference from your person. Therefore, do not wear the following:
- Necklaces or any other jewelry
- Antiperspirant or deodorants underneath your arms
- Talcum or baby powder, or lotions on your breasts or armpits
What's a ductogram like?
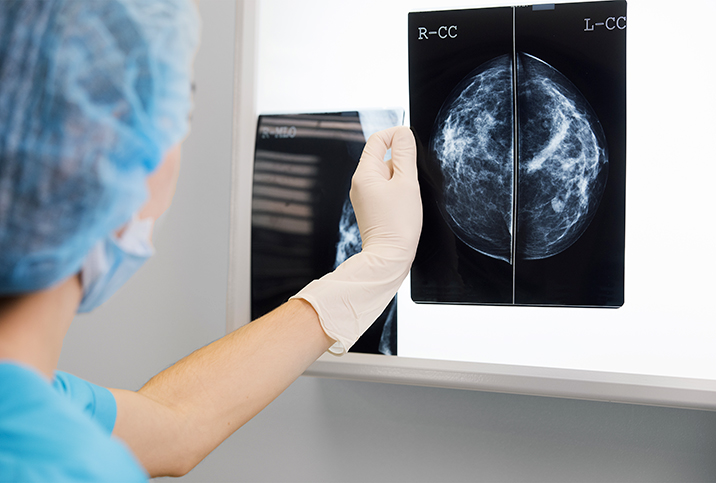
A ductogram can be performed in a radiology clinic or a hospital and will take roughly 20 minutes to 1 hour. Since a ductogram requires the milk ducts to be dilated, the experience may cause some discomfort. However, you need not worry—generally, the procedure is not painful.
The objective of the radiologist, the doctor who reads the images from a ductogram, is to look for a possible "filling defect" on the mammogram.
"If there is anything suspicious growing in that duct (which is the greatest concern with single duct nipple discharge), we will see contrast filling the duct and what we call a filling defect on the mammogram," Chan said.
Reitherman discussed the steps to expect during a ductogram procedure:
- First, the patient is asked to remove all clothing from the waist up and to change into a gown.
- The patient will lie on her back, and a small gauge catheter or cannula is gently inserted in the duct from which the discharge is emanating.
- Then a small amount of radio-opaque contrast dye is gently injected by a technologist to fill the ductal system from which the discharge is arising.
- From the X-ray image, your doctor will be able to see its shape and observe possible concerns like lumps within the ducts.
- Mammograms are then performed. You will be asked to stand in front of the mammogram equipment. Two plates may flatten the breasts to obtain a clear image of the ducts. The contrast material fills the duct and will detect any filling defects or other aberrations that may indicate underlying pathology.
- The radiologist will read the images and evaluate their clarity. If the pictures obtained aren't clear, you may need to re-do the test.
It is helpful to note there are limitations to the ductography procedure.
"I always want my patients to know that not all ductograms are successful," Chan warned. "If we cannot isolate the responsible duct, then we won't place the cannula or inject the contrast. If we are able to, you may expect to feel some pressure from the cannula and the contrast."
"If a ductogram cannot be performed for technical reasons, a breast MRI is an excellent imaging procedure that can provide the necessary information for possible surgical intervention," Reitherman added.
Next steps
Your doctor will call you with the final results of the ductogram, and then discuss if surgery is recommended or if additional tests are needed.
"A breast MRI with and without contrast may be recommended," Chan said. "This is a great way to look at subtle findings that may not show up on mammography or ultrasound."
Reitherman said a breast MRI may be utilized whether the ductogram is positive or negative to provide information on whether surgery is needed.