Women Should Start Screening Mammograms at Age 40

Key Points
- Breast cancer claims thousands of lives every year. Screening mammograms can help find breast cancers early when the disease is more treatable.
- A major United States task force updated its screening recommendations, advising people with an average risk of breast cancer to start getting mammograms at age 40 instead of 50.
- The new recommendation is intended to encourage more people to get tested earlier and make screenings more accessible.
The United States Preventive Services Task Force (USPSTF) released draft recommendations back on May 9, 2023, with guidelines for breast screening.
On Tuesday, April 30, 2024, the task force updated those guidelines, which now recommend women and people assigned female at birth (AFAB) who have an average risk of breast cancer to begin getting mammograms at age 40 — and screened every other year until they're 74.
That's a decade earlier than the independent expert panel's previous recommendation to begin screening for breast cancer at age 50.
What are the current guidelines for mammogram screening?
Recommendations for when you should get a mammogram vary among organizations.
The American Medical Association (AMA) recommends women at average risk for breast cancer receive their first mammogram at age 40, for example. At the same time, the American Cancer Society (ACS) recommends beginning mammograms at age 45.
“Many, however, have already advised people to consider starting screening mammograms at age 40,” said Maryam Lustberg, director of the Center for Breast Cancer at Yale Cancer Center and Smilow Cancer Hospital in New Haven, Connecticut.
Since 2009, the U.S. Preventive Services Task Force has recommended those at average risk start screening for breast cancer at age 50. In 2016, the organization updated its guidelines to say women could start getting mammograms at age 40 but that patients should make an individualized decision.
"This official change by USPSTF hopefully will bring additional awareness about the importance of timely screening and that younger women can get breast cancer," Lustberg said.
Organizations' guidelines are different for people at high risk of breast cancer.
The ACS, for example, recommends women and AFAB people who have risk factors such as the BRCA gene or a family history of the disease begin having mammograms at age 30.
Women with risk factors such as dense breasts, Black ethnicity, an early age of menstruation, a history of chest or face radiation or smoking may also want to start screening earlier.
Although Black women are as likely as people of other ethnicities to develop breast cancer, they're more likely to develop aggressive forms of the disease at a younger age and more likely to die, according to Breastcancer.org.
Similarly, medical experts and organizations, including the USPSTF, recommend people with a personal history of breast cancer and other high-risk factors screen more frequently than their peers.
Recommended
- Should You Be Tested for the BRCA Mutation?: The 'cancer gene' might be new to your knowledge base, but learning more about the cancer gene can only help.
- Why Is Breast Health Important?: From breast cancer to breastfeeding, here's why breast health is crucial to women's health.
- 5 Things Every Man Should Know About Male Breast Cancer: With so much focus on breast cancer in women, too many cisgender men aren’t aware of the risks.
Why did the recommendation for when you should get a mammogram change?
The U.S. Preventive Services Task Force systematically analyzes evidence and provides recommendations. After reviewing data from several large studies, they determined that mammograms every other year provide a "moderate net benefit" for people ages 40 to 74 with an average risk of breast cancer.
The panel had previously believed that, for people under 50, the risks of mammograms—including radiation exposure, unnecessary biopsies and anxiety-inducing false positives—outweigh the benefits.
The panel concluded that there is not enough evidence to recommend routine screenings for women and AFAB people ages 75 and older.
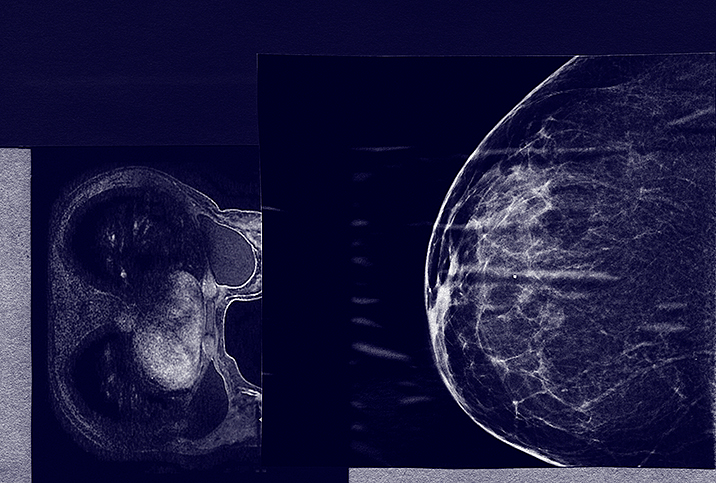
They also decided not to endorse supplemental screening methods, such as MRIs and ultrasounds, for all people with dense breasts. The task force noted that healthcare professionals should make individualized decisions about how to screen for people in these groups.
The change could be vital for thousands of people, according to various medical organizations including the American College of Obstetricians and Gynecologists (ACOG), which have released statements responding to the update.
Unlike breast self-exams, mammograms are an important tool to find breast cancers early when they are more easily treatable.
"With my own experience of being diagnosed with breast cancer at a young age, plus new data showing that more younger women are being diagnosed with breast cancer, I think this is such an important step to raise awareness and help this become a standard recommendation for screening," said Anne Peled, M.D., a breast cancer and plastic and reconstructive surgeon based in San Francisco.
"I have seen many women in my practice get diagnosed with early-stage and very treatable breast cancer from a screening mammogram in their early 40s, which is a great example of how mammograms can be lifesaving," Peled said.
The new screening recommendations could also make mammograms more accessible, Peled said. The USPSTF assigns grades to various preventative healthcare services, which are used to determine if insurers must cover them under the Affordable Care Act.
The task force assigned a "B" grade to screening mammograms for people ages 40 to 74 with average breast cancer risk. Insurers have to cover services with "A" or "B" grades.
"Having the USPSTF guidelines officially published should eliminate any barriers for people getting mammograms starting at age 40," she said.
"While some other organizations had already recommended starting screening at age 40 and clinicians have been able to order mammograms for patients in their 40s and get insurance coverage previously, officially updated guidelines will hopefully encourage more providers to order mammograms without concerns around coverage," Peled finished.
How do you know when you should get a mammogram?
"Knowing your risk factors is the first step to deciding if you want to start getting screening mammograms before age 40," Lustberg said. "Talk to your healthcare provider for individualized guidance if you're in a high-risk category."
"People with higher-than-average breast density may also want to consider additional screening beyond mammograms," Peled added.
If getting to a doctor's office is a hurdle, see if any mobile mammography providers serve your area. Hospitals and healthcare networks increasingly provide such services, including in rural areas.
Some people diagnosed with breast cancer report having detected a lump through a self-exam. Guidelines vary, but several organizations suggest doing these monthly in the week before your period, according to Cleveland Clinic.
Although medical opinions vary on the importance of a self breast exam, it could help you identify changes that may warrant a visit to your healthcare provider, who can order a mammogram or MRI if necessary.
"Even though it can be scary to get mammograms, most screening mammograms end up being normal," Peled said.
"In the rare chance that they do end up finding breast cancer, it would almost certainly be at an early stage and small size where more treatment options and better outcomes would be possible as a result of having done the screening."
The bottom line
Breast cancer is a leading cause of death among women and AFAB people in the United States, but malignancies are highly treatable when detected early.
Talk to your healthcare provider to determine your risk of breast cancer and the best time to start screening.