Menopause and Breast Cancer: What Is the Relationship?

If you're approaching menopause and are wondering how that affects your risk of breast cancer, you're not alone. We spoke to leading physicians to find out what women in the menopausal transition need to know about their breast cancer risk.
Why does breast cancer risk increase as you age?
Menopause does not cause cancer. However, your risk of developing cancer, including breast cancer, does increase the older you get.
"Cancer is a disease of aging, meaning that the majority of cancers occur in older individuals. Various reasons contribute to that. Our normal cells change as we age, and their DNA might acquire genetic damage that we are unable to repair. This includes breast cancer," said Chadi Nabhan, M.D., an oncologist and the senior vice president of Caris Life Sciences in Chicago.
The longer one is exposed to estrogen, the higher their risk.
For breast cancer specifically, excess estrogen exposure has been linked to an increased risk, according to Nabhan, who is also the host of the podcast "Healthcare Unfiltered" and author of "Toxic Exposure: The True Story Behind the Monsanto Trials and the Search for Justice." The longer one is exposed to estrogen, the higher their risk. The older a woman is when she reaches menopause, the higher her risk of developing breast cancer can become because she has been exposed to estrogen longer.
On the other hand, "early menopause, due to decreased exposure of endogenous hormones, likely decreases lifetime breast cancer risk, yet increases the risk of cardiovascular disease," said Robin Noble, M.D., a board-certified gynecologist in Portland, Maine, and the chief medical advisor for Let's Talk Menopause, a national nonprofit organization.
In addition to estrogen exposure and age at menopause, other risk factors contribute to a person's risk of breast cancer—some controllable and some not.
According to Noble, these risk factors can include:
- Having your first child after the age of 30
- Obesity
- Alcohol intake
- Sedentary lifestyle
- Dense breast tissue (breasts that have more glandular, fibrous or connective tissue)
Factors that are linked to decreased breast cancer risk include:
- Earlier childbearing
- Breastfeeding or pumping
- A diet low in saturated and animal fats
- Regular exercise
However, it's important to put these additional risk factors in perspective.
"The two biggest risk factors that any woman has for developing breast cancer remain, one, having breasts, and two, living long enough to get breast cancer," said Lori Alfonse, D.O., surgical oncologist and deputy physician in chief at Lehigh Valley Topper Cancer Institute in Bethlehem and Allentown, Pennsylvania.
Can hormone therapy potentially cause breast cancer?
One way to relieve menopausal symptoms such as hot flashes, osteoporosis and vaginal dryness is with menopausal hormone therapy (MHT), also called hormone replacement therapy (HRT) and menopausal hormone replacement therapy (MRT).
There is a lot of mixed messaging about the risks of hormone therapy, specifically related to breast cancer. This is largely due to the Women's Health Initiative, a large study whose findings and methodology have since been questioned. It suggested that women who took combined hormone therapy (estrogen and progestin) had a higher risk of breast cancer and blood clots.
However, research in the decades since suggested that the relationship between hormone therapy and breast cancer is complex and not as clear-cut as once thought, according to BreastCancer.org, a nonprofit organization that provides educational content on breast cancer.
"Estrogen plus progestin seems to increase the risk of breast cancer slightly—from 23 out of 1,000 cases in women ages 50 to 59 over a five-year period, to 27 out of 1,000 cases," Noble said. "This increase is far less than the increase seen [from] obesity or moderate alcohol consumption."
Meanwhile, estrogen-only MHT may help potentially decrease the risk of breast cancer, osteoporosis and colon cancer, a 2020 study suggested.
However, it's important to note that estrogen-only hormone therapy should only be prescribed to women who have had a hysterectomy because it is associated with an increased risk of endometrial cancer. A combination of estrogen plus progestin is not, according to the National Cancer Institute.
"The American Cancer Society (ACS), as well as the Women's Health Initiative (WHI), says estrogen-only HRT is not linked to a higher risk of breast cancer," Alfonse said.
Does the length of time you take MHT contribute to a future breast cancer diagnosis?
When it comes to combination MHT, the length of time a person is on it and the dosage matter. It's why MHT isn't typically prescribed for women over age 60.
"The risk of breast cancer associated with MHT/HRT use appears to be related to both the duration of treatment and the type of hormones used. Women who use MHT/HRT for longer periods of time are at greater risk, as are those who use combination therapy (estrogen plus progestin) as opposed to estrogen alone," explained Melanie Bone, M.D., an OB-GYN in Palm Beach, Florida, and the U.S. medical director of Daye, a gynecological health company.
The data, according to Bone, indicate benefits for HRT/MHT in low-risk women for five years at the onset of menopause. After that, any decision regarding its continuation should be made between the patient and the clinician.
"It is commonly accepted that menopausal hormone replacement therapy (MRT) for less than five years does not pose an increased risk of breast cancer development," Alfonse said. "Higher-dose combination MRT increases breast cancer risk more than lower-dose combination MRT. Combination MRT also increases the likelihood that the cancer may be found at a more advanced stage and is often linked to increased breast density, which can make it harder for mammograms to detect breast cancer."
Deciding whether to use hormone therapy requires patients to put the risks into perspective, weigh the pros and cons and be aware of their risk factors, such as a family history of breast cancer. Women and their physicians can decide how to best manage menopausal symptoms.
"The risk of breast cancer associated with MHT/HRT must be balanced against the potential benefits of treatment, which can include relief of menopausal symptoms and a reduced risk of osteoporosis and fractures," Bone said. "Women considering MHT/HRT should discuss the potential risks and benefits with their physicians and make informed decisions based on their individual circumstances."
How can you reduce your risk of breast cancer?
Being proactive is key to protecting yourself from breast cancer.
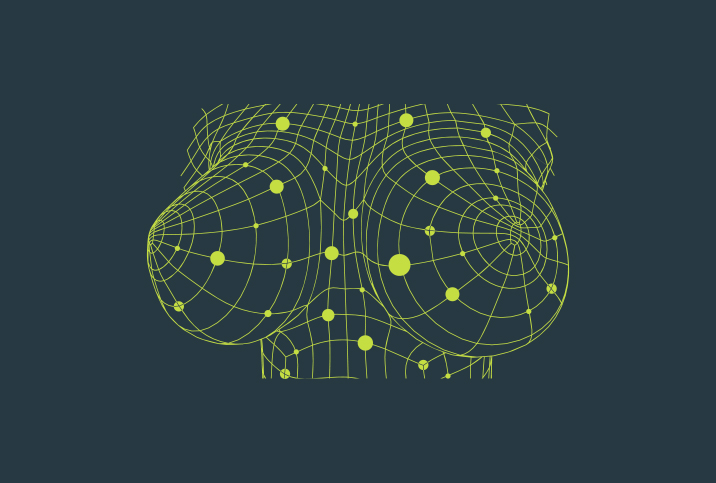
Breast awareness is important, according to Noble. If you notice any changes in your breasts, you should notify your healthcare provider.
Look for changes in your breasts, such as:
- Asymmetric pain
- Nipple discharge
- A mass or lump
- Skin changes
- Contours, nipple inversion or other shape changes
"Appropriate breast cancer screening and breast self-exam (BSE) remain the two most important ways that women can remain vigilant about breast cancer detection," Alfonse said.
Women with an average risk of breast cancer should receive a mammogram every one to two years beginning at age 40, Noble said.
"Higher-risk women will likely be in protocols that incorporate clinical breast exams with alternating mammograms and breast MRI at six-month intervals," Noble added.
"Regular breast cancer screening is also important for women who use MHT/HRT," Bone added. "Excitingly, novel AI technologies are now able to detect breast cancer at exceptionally early stages, encouraging early treatment and better patient outcomes."
The bottom line
Know your body, maintain a healthy lifestyle and stay physically active to help improve your general wellness. Schedule the exams you need according to your risk as determined by your doctor.
If you are experiencing any side effects of menopause, talk to your doctor to determine the best course of action.