Understanding Treatment for Hypospadias and Its Complications

Hypospadias is a relatively common birth defect in which the opening of a boy's urethra, the hole that urine and semen pass through, isn't located in the usual spot at the end of the penis.
About 1 in 200 boys are born with hypospadias, according to the Centers for Disease Control and Prevention (CDC).
With hypospadias, the opening to the urethra can be located anywhere from just below the head of the penis to somewhere along the shaft or even on the scrotum or perineum. While the exact cause is unknown, it's thought to be due to a combination of genetic and environmental factors.
For instance, mothers who are age 35 or older and considered obese are more likely to have babies with hypospadias. Exposure to fertility drugs, certain hormones, and possibly plastics and pesticides may also be contributing factors.
How is hypospadias treated in infants?
Hypospadias treatment depends on the individual case. Sometimes, the location of the opening of the urethra is deemed "close enough" to the end of the penis that it shouldn't cause the person too much difficulty with urination or fertility issues.
"It depends on where the opening is," said Amy Pearlman, M.D., a men's health specialist and co-founder of Prime Institute in Fort Lauderdale, Florida. "Not all hypospadias needs to be repaired. So if the opening is coming out kind of by the tip but a little bit lower, it's kind of up to the parents honestly if they want to get it fixed."
If the opening is located farther down the penis shaft or on the scrotum, surgical repair is often the best choice. If surgical repair is needed, doing so during infancy is usually recommended, typically when the boy is between 6 months and 2 years old.
Depending on the severity of the hypospadias, it may require more than one surgery to repair.
Most boys who are born with hypospadias, whether or not they have repair surgery, manage to live full, complete lives with only minor inconveniences or other issues.
Parents who elect to have their child circumcised generally have it done within days of birth. If their baby has hypospadias, that could change. Healthcare providers usually recommend babies born with hypospadias have their foreskin left intact, if possible, at least until it's time to perform the repair. That's because the foreskin itself is often used in repair surgery.
A surgeon will use a piece of the foreskin or other tissue to create a tube and lengthen the urethra to allow it to open at the end of the penis. They may sew a catheter in place to help the newly created tube hold its shape while it heals, which will need to be removed a week or two later.
"So you kind of create wings on either side, and then you kind of tubularize the tissue over a small stent or catheter," Pearlman said. "A lot of these surgeries are done in kids while they're still developing. So their anatomy is very tiny, so we're using very small sutures and loupes that magnify the field."
How is hypospadias treated in adults?
If the hypospadias is severe enough to warrant surgery, the preference is, again, to do the repair during infancy. However, it is possible to surgically repair hypospadias in adulthood, although it is a more complicated and difficult procedure.
In fact, many adult men who have undergone hypospadias repair may require subsequent surgeries to address complications that develop as they age. One study found that hypospadias repair candidates required an average of three surgeries; 10 percent of these men required five or more surgeries.
Physical complications of hypospadias treatment
Even successful hypospadias repair patients frequently experience physical complications involving urination. These may include the following:
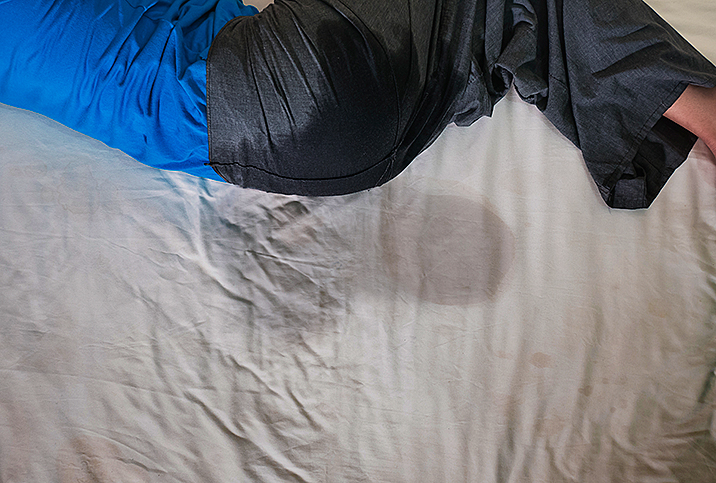
- Post-urination dribbling
- Deviation of the urinary stream
- Surplus of skin
Other, more severe complications can arise over time—even a decade or more later. Scar tissue can form, as can fistulas, which are new openings in the skin that aren't supposed to be there. Sometimes, the new urethral opening may close as the child develops, a condition called urethral stricture.
A vast majority of hypospadias repair surgeries are successful and last a lifetime.
"The further back the opening is, the higher likelihood of complications," Pearlman said. "That area can scar down, and it can cause fistulas—abnormal connections between the urethra and the skin where they leak in a different area. I see some of those guys when they become adults because they have scar tissue, or they have fistulized, or they have curvature of the penis. Often with hypospadias, they have curvature they were born with, and it's down toward the feet."
Psychological complications of hypospadias treatment
Surgery—or surgeries—in such a sensitive area causes a lot of trauma. Given that, it should come as no surprise that men and boys who have hypospadias may suffer some psychological issues. If they have ongoing urinary issues that force them to sit down to pee, that can make boys feel as though they're different.
Some men may also develop dissatisfaction with the appearance of their genitals, which can lead to other complications. One long-term study found that a majority of hypospadias repair recipients had poor genital perception, which was correlated with low self-esteem in general. (This was a very small study with only 77 participants, so it shouldn't be considered conclusive.)
Another small study found that men who had undergone hypospadias repair had higher rates of urinary dysfunction and sexual dysfunction. Fortunately, numerous support groups exist for men who have hypospadias, and online documentation can help them learn how to better live with the condition.
Prognosis
A vast majority of hypospadias repair surgeries are successful and last a lifetime. However, as outlined above, the potential for complications is real, including fistulas and scarring that can divert urine flow. Keeping a close eye on the boy's development and promptly addressing any issues that might come up can help ensure he gets any subsequent treatments he might need in a timely fashion.
Helping to monitor and support the mental health of a person with hypospadias may help prevent some of the worst potential psychological complications.
The takeaways
Hypospadias is a relatively common birth defect. The good news is this means the surgical techniques and recovery protocols are well-developed and very successful simply due to being used so frequently.
Most boys who are born with hypospadias, whether or not they have repair surgery, manage to live full, complete lives with only minor inconveniences or other issues.
Their urethral opening may not be at the end of the penis, but it's not the end of the world.