What Are the Early Signs of Cervical Cancer?

Cervical cancer can be deadly. Early detection significantly increases your chance of survival. Knowing the risk factors and signs can make all the difference for you and your loved ones.
What are the early signs and symptoms of cervical cancer?
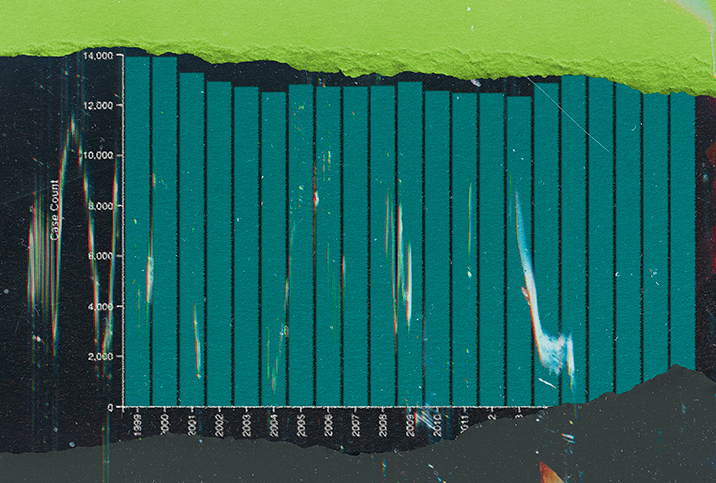
Nearly 14,000 women will be diagnosed with cervical cancer in 2023, according to the American Cancer Society. While that figure may be a little scary, it's not a death sentence for most women—at least when caught early.
The five-year relative survival rate of the disease is 91 percent if diagnosed early, according to the National Cancer Institute.
The real problem is that cervical cancer isn't immediately noticeable. Not every woman understands the symptoms of cervical cancer—and skipping women's health screenings doesn't help.
"Unfortunately, early-stage cervical cancer may not be symptomatic," said Clare Bertucio, M.D., a radiation oncologist with Peninsula Radiation Oncology Center in Soldotna, Alaska, and CEO of Medicine Mama's Apothecary.
"Some signs of cervical cancer include pain or vaginal bleeding following intercourse or outside the usual menstruation window," said Laura Purdy, M.D., a Nashville-based family medicine physician.
You may notice watery or bloody discharge, Purdy said.
Some of the symptoms of cervical cancer can signify other problems, too, such as vaginismus, a yeast infection or pelvic inflammatory disease.
"While none of the above [symptoms] are a diagnosis of cervical cancer, they are abnormal and should be evaluated by your healthcare provider as soon as possible," Bertucio said.
She urged getting regular Pap smears, as well.
"As a radiation oncologist, I cannot stress enough the benefit of early detection and intervention in terms of outcomes," she said.
Recommended
- Can You Get Cervical Cancer if You Don't Have Sex?: HPV causes most cervical cancer cases, but a small risk exists for people who aren't sexually active.
- More Cases of Cervical Cancer Linked to HPV Than Previously Thought: A new study reaffirms a strong link between this gynecological cancer and human papillomavirus.
- HPV Vaccine Substantially Reduces Cervical Cancer Rates: Countries with high HPV vaccination rates 'on the path to eliminating cervical cancer,' experts say.
How is cervical cancer diagnosed?
Cervical cancer screenings can consist of three tests (though you probably won't get all three) that have one thing in common: tissue sampling.
"This may be through a simple screening Pap test or more invasive procedures, like [a] biopsy," said Aldene Zeno, M.D., founder of Essence Health and Urogynecology in California.
"In low-resource settings, advanced cancers are diagnosed clinically based on appearance during [a] pelvic exam," Zeno said.
Some people may already know what a Pap smear feels like: It's a mildly uncomfortable procedure in which a doctor gets cells from your cervix by putting a swab into your vagina. A pelvic exam is similar—a doctor looks and feels around internally and externally.
A cervical biopsy, however, entails the removal of tissues or treatment of cells through a blade, scalpel or similar instrument, in which you may be numbed or given anesthesia.
It's important to note that the pelvic exam or Pap smear may come first but probably won't be last. A cervical biopsy is required for an official diagnosis, Purdy said.
What are the risk factors of cervical cancer?
Cervical cancer risk factors are many—smoking, herpes, age, HIV and a weakened immune system, for example—but the main cause is the human papillomavirus (HPV).
HPV is the most common sexually transmitted infection (STI) in the United States, according to the Office on Women's Health (OASH), although it can also be spread through skin-to-skin contact.
The human papillomavirus causes 95 percent of global cervical cancer cases, according to the World Health Organization (WHO).
There is good news. Cervical cancer can be prevented.
The primary way to prevent the disease is the HPV vaccine, such as Gardasil, Gardasil 9 or Cervarix.
All 11 to 12-year-olds of any gender should consider getting the vaccine, per recommendations by the Centers for Disease Control and Prevention (CDC). If you're between ages 27 and 45 and haven't gotten this shot, discuss your options with your doctor.
"The current Gardasil vaccine protects against nine types of high-risk HPV infection, including the most common types, HPV 16 and 18," said Jill H. Tseng, M.D., a gynecologic oncologist with Providence St. Joseph Hospital in Orange County, California.
While it's highly effective as a preventative measure, she said, it doesn't limit your risk exposure entirely.
Stay safer while having sex. Oral, vaginal or anal, the type of sex doesn't matter when it comes to limiting your HPV exposure risk—and it doesn't matter if the person has symptoms or not, according to the CDC.
HPV can still be spread. Avoid touching HPV warts. Wearing condoms can help reduce the risk of passing HPV, but it doesn't completely eliminate the chance.
Schedule your routine Pap smear every three years or per your trusted doctor's recommendation.
"It is important to stay up-to-date with these screenings because they allow for your doctor to catch it as early as possible so that [it] can be intervened if you are in the early stages of developing cervical cancer," Purdy said.
How is cervical cancer treated?
Cervical cancer treatment looks different for each person depending on how far along the cancer is, so a doctor will carry out various tests.
"Once diagnosed, a woman undergoes a thorough staging work-up, which includes a comprehensive physical exam, perhaps an examination under anesthesia (this allows a more extensive ability to view the cervix and surround[ing areas], without [causing] unnecessary discomfort), a CT and sometimes even a PET scan," Bertucio said.
If the cancer is just in the cervix, a hysterectomy, or the surgical removal of the uterus, or a radical hysterectomy (a hysterectomy plus the removal of your cervix, ovaries, fallopian tubes and nearby tissues) and sampling of the lymph nodes in the pelvis is usually the process, Tseng said.
You'll typically receive anesthesia for the hour-long procedure.
In the early stages, some people can get a trachelectomy (the cervix, upper vagina and tissues surrounding the cervix are removed) if they want to be able to get pregnant after treatment.
"For more advanced disease that spreads outside the uterus, treatment consists of radiation, chemotherapy or a combination of both," Tseng said. Immunotherapy may be included.
The bottom line
As tempting as it may be, don't skip out on Pap smear exams. If you are under the age of 45 and haven't had the HPV vaccination, schedule yours today. Talk to a doctor if you notice any abnormal symptoms during or after sex or your period.