Should You Be Tested for the BRCA Mutation?

If you’ve heard of the BRCA1 and BRCA2 gene mutations, you likely have Angelina Jolie to thank. BRCA1 and BRCA2 were first identified a little more than 25 years ago, but awareness of the mutations has exploded only in recent years. A look at Google Trends shows that search interest for the term “BRCA mutation” nearly quadrupled between 2004 and present day. Interest peaked in May 2013, which happens to be the same month Jolie announced she had undergone a preventive double mastectomy after being diagnosed with the BRCA1 gene mutation.
Despite this spike in awareness, though, many misconceptions still surround the BRCA gene mutations, according to Eleanor Griffith, a certified genetic counselor and founder of Grey Genetics. While more people have heard of the BRCA mutations and how they increase the risk of certain cancers, they don’t necessarily know who is susceptible to the mutations, how to get tested and what to do with a confirmed diagnosis.
Defining the BRCA1 & BRCA2 mutations
To start, let’s clarify: The mere presence of BRCA1 and BRCA2 genes is nothing to worry about. In fact, they’re the good guys. The two genes, which everyone has, play an important role in suppressing cancer and other diseases. Rather, the presence of BRCA1 and BRCA2 mutations is cause for concern.
“Mutations, or pathogenic—harmful—variants in genes keep them from working normally,” Griffith said. “In the case of the BRCA1 and BRCA2 genes, pathogenic variants confer an increased risk for several types of cancer.”
Griffith noted there is a slight difference in the estimated risks for cancer with pathogenic variants in BRCA1 versus BRCA2. “But they’re similar enough that they are usually discussed together,” she said.
Jillian Barberie, TV host and breast cancer survivor, discusses her road to diagnosis and treatment, which came after a previous negative BRCA mutation test. Watch the full interview here.
Somewhere between 1 out of 200 and 1 out of 500 people has these mutations. Although they are often thought of as a “woman’s issue,” Griffith said they are just as common in men, and both sexes are equally likely to pass the mutations to their children.
Another misconception is that only people of Ashkenazi Jewish heritage carry BRCA mutations.
“BRCA mutations are found in all different populations, not just those of (Ashkenazi Jewish) ancestry and not just white women,” Griffith said.
Associated health risks
Although the BRCA mutations are not present in a majority of breast and ovarian cancer cases, women with a BRCA mutation are significantly more likely to be diagnosed with those diseases. A 2017 study of women diagnosed with a BRCA mutation found that about 72 percent of BRCA1 mutation carriers and 69 percent of BRCA2 mutation carriers developed breast cancer by age 80, while 44 percent of BRCA1 mutation carriers and 17 percent of BRCA2 mutation carriers developed ovarian cancer by age 80.
Men with BRCA mutations face an increased risk of breast cancer as well, although it’s significantly smaller: lifetime risk of diagnosis is 1 percent for BRCA1 mutation carriers and 7 to 8 percent for BRCA2 mutation cancers. Men with these mutations also face an increased risk of prostate cancer: 3.4 percent for BRCA1 mutation carriers and 5.2 percent for BRCA2 mutation carriers.
Although the BRCA mutations are not present in a majority of breast and ovarian cancer cases, women with a BRCA mutation are significantly more likely to be diagnosed with those diseases.
Both male and female carriers of the BRCA mutations carry an increased risk for pancreatic cancer, melanoma and Lynch syndrome, which Griffith said is associated with “high risks of developing colon and uterine cancers, significantly increased risks for stomach and ovarian cancer, and more modestly increased risks for a number of other cancers.”
“Although Lynch syndrome receives much less public attention than hereditary breast and ovarian cancer, it is just as common,” Griffith added, “affecting between 1 out of 200 and 1 out of 500 individuals in the general population.”
Populations at risk for BRCA mutations
Anyone with a family history of BRCA- or Lynch syndrome-related cancers—particularly at a young age—has a high risk of carrying the mutations, as do individuals with Ashkenazi ancestry. In addition, according to Griffith, “Some studies have shown that there is a higher prevalence of BRCA mutations among Black women specifically.”
People of all different demographics and backgrounds can carry BRCA mutations, though, so don’t rule it out entirely—even if your healthcare providers do. Griffith said that even among professionals there are misconceptions that only individuals of certain backgrounds can be carriers.
People of all different demographics and backgrounds can carry BRCA mutations.
“Sometimes…healthcare providers think that if someone is not of (Ashkenazi Jewish) ancestry, they can’t have a BRCA mutation,” Griffith said. “This misinformation can keep people from being referred to genetic counseling and/or offered testing by their healthcare providers when it would be appropriate.”
Griffith pointed to Black women as an example.
“Black women are less likely to be referred to genetic counseling and less likely to be offered genetic testing by their healthcare providers, (and that only)exacerbates existing health disparities,” she said.
How BRCA mutation testing works
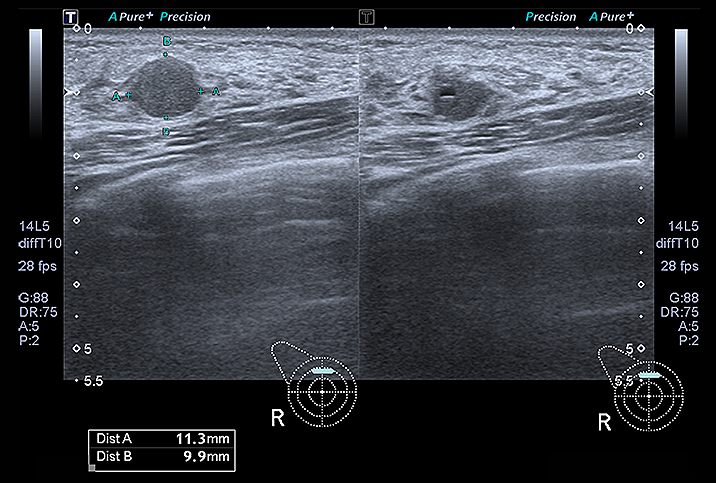
Medical professionals will test DNA from blood or saliva samples. Griffith explained that this is a two-step process: The genes must first be analyzed and then interpreted.
Because of differences in quality and interpretation between labs, Griffith recommends people use a genetic counselor to help them understand their family history, testing options and test results. She also cautioned against direct-to-consumer tests, such as 23andMe, which test only for a certain number of possible BRCA mutations when thousands exist.
A majority of insurers, along with Medicaid, will cover BRCA mutation testing only if you meet certain criteria dictated by the National Comprehensive Cancer Network, such as having a blood relative with a known mutation or having a family history of certain hereditary cancers diagnosed at young ages. Medicare guidelines are stricter, requiring someone to have had a personal diagnosis of a BRCA-related cancer. For people who don’t meet the criteria, tests may be available for a “few hundred dollars out of pocket,” according to Griffith.
Understanding your results
A negative test result is definitely good news, but if you have a significant family history of BRCA-associated cancers, you may want to pursue further testing. Even if you have a positive result, though, Griffith said there are many different medical management options available. Depending on your specific type of gene mutation, personal medical history, family medical history and other circumstances, doctors may recommend prophylactic surgeries—the choice Angelina Jolie opted for—enhanced disease screening protocols or even just waiting to see how things develop.
Whatever the result of your test, the information you learn can benefit your present and future health.