How is Endometrial Cancer Treated?

Endometrial cancer is the most common gynecological cancer in American women. There are two kinds of uterine cancer: endometrioid and non-endometrioid. Although this cancer can affect women of all ages, most patients are diagnosed after age 50. If you have noticed bleeding between periods or minor spotting after menopause, talk to your doctor.
Early detection is the most powerful way to improve your odds of overcoming endometrial cancer. Once diagnosed, your doctor will discuss your next steps. Your treatment will likely include a combination of the treatment options below.
How do you treat uterine cancer?
Uterine cancer isn’t uncommon. In 2023, an estimated 66,200 women will receive a positive endometrial cancer diagnosis, and about 13,030 women will die from the disease. However, there are more than 600,000 survivors. Detection in the early stage and beginning proper treatment are important.
"Treatment depends on several factors, including the cell type of the endometrial cancer and the woman’s fertility goals," said Evelyn Fleming, M.D., a gynecologic oncologist at Dartmouth Hitchcock Medical Center in Lebanon, New Hampshire.
Surgery
Beyond removing the cancer, surgery gives your doctor critical information about if and where the cancer has spread. "Staging" your cancer (Stage I through Stage IV) guides the medical team’s recommendations for your next steps, Fleming said.
Surgery is the standard first-line treatment for endometrial cancer. This treatment includes removing the uterus (hysterectomy), plus the fallopian tubes and ovaries (salpingo-oophorectomy). A hysterectomy eliminates any chance of future pregnancy.
Regardless of age, having your ovaries removed will also trigger menopause. Some younger women with early-stage cancer opt to keep their ovaries to prevent menopause.
Although surgery is the gold standard for treating endometrial cancer, patients who want to get pregnant in the future do have options, Fleming stated. The risks and benefits of these choices should be thoroughly discussed with your doctor.
Hormone therapy
Hormonal therapy could sometimes be a treatment option for young patients who want the ability to have a baby in the future, Fleming said. Progesterone has long been used as a treatment therapy for endometrial cancer.
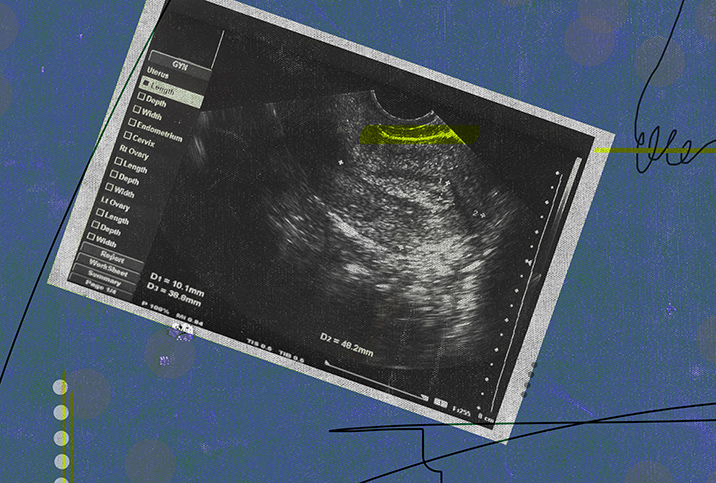
Hormone therapy works by slowing the development of endometrial cancer cells. An intrauterine device (IUD) that secretes progesterone directly into the uterine lining, for instance, can be used to treat precancerous endometrial hyperplasia or even early-stage cancer, Fleming explained.
While research is ongoing, ACS states that at this time, no one hormone treatment is considered the best way for endometrial cancer. Your doctor might recommend combining more than one hormone drug or using hormone therapy with chemotherapy.
"This approach requires careful monitoring and is best done with a gynecologic oncologist, the doctor who is specially trained in women’s cancer care," Fleming cautioned.
Radiation
Radiation therapy uses intense energy beams to kill cancer cells. This cancer treatment can be administered from outside or inside your body. Radiation is usually used after surgery to kill any remaining cancer cells. Sometimes radiation is used to shrink a tumor before surgery.
Internal radiation therapy, called brachytherapy (BT), places a small radioactive device inside the vagina. A 2011 research review published in Current Oncology Reports suggested internal radiation produced less severe bowel-related side effects than external radiation therapy.
During external radiation therapy, you’ll lie flat on a table while the doctor uses a machine to focus energy beams on the cancer-affected area. In most cases, radiation is a supplementary cancer treatment. More rarely, patients who aren’t healthy enough for surgery use radiation as their primary treatment against endometrial cancer.
Medical professionals consider your overall health and cancer stage when deciding whether to recommend radiation therapy and the type of radiation.
Chemotherapy
Chemotherapy, or chemo, involves using chemicals to kill cancer cells. Some chemo is offered in pill form, while some are given intravenously (with in-office IV treatments).
Not every endometrial cancer patient needs chemotherapy, according to the ACS. It’s typically recommended as a secondary (post-op) treatment for advanced or aggressive cancers, such as those in stages III and IV.
Like radiation therapy, chemo is sometimes recommended to wipe out any remaining cancer cells after surgery. It’s also occasionally used to shrink tumors before surgery.
Targeted drug therapies
Targeted drug treatment is an umbrella term for drugs targeting weaknesses in specific cancer cells to encourage the cells to die off. Some medications are given in pill form, while others are administered through an IV.
This is a newer way of treating endometrial cancer, according to the ACS, and is often paired with chemo or immunotherapy.
Immunotherapy
Immunotherapy refers to drug treatments that strengthen your body’s ability to fight disease. This treatment stimulates your immune system in a very specific way so that it’s more primed to go head-to-head with endometrial cancer cells.
In 2021, the Food and Drug Administration (FDA) approved Dostarlimab (Jemperli), an immunotherapy treatment for recurrent or advanced endometrial cancer. It can help the body fight against specific endometrial cancer cells, but it’s not a fit for every case.
Can endometrial cancer be prevented?
Endometrial cancer is not 100 percent preventable, but there are several ways to reduce your risk. Regular physical activity is one of the best ways to reduce your risk.
Fleming said most endometrial cancer cases are associated with obesity—a body mass index (BMI) of 30 or above.
"Exercising regularly and maintaining a normal BMI can help prevent endometrial cancer," she added.
People with a family history of endometrial or colon cancer can get genetic testing to check for Lynch Syndrome, a common inherited cause of endometrial cancer. If a patient has Lynch Syndrome, Fleming recommends risk-reducing surgery—removing the uterus, fallopian tubes and ovaries—once pregnancy is no longer desired.
If you experience chronic irregular cycles, it’s important to pinpoint and treat the cause to minimize your endometrial cancer risk, Fleming said. Hormone imbalances or fluctuations that lead to excess estrogen exposure gradually increase your odds of developing this type of cancer.
The bottom line
Endometrial cancer isn’t entirely avoidable, but with certain lifestyle modifications, you could help reduce your risk. If you experience unusual symptoms, such as bleeding after menopause, or have a family history of endometrial cancer, speak with your doctor.
If you need a new doctor, Giddy Telehealth can provide a one-stop-shop. With access to hundreds of healthcare professionals, it’s a convenient way to find your new doctor. Many offer video consultations and same-day appointments.
Regardless of how you get seen, taking that step is a critical part of the battle because, as with many other forms of cancer, early diagnosis and prompt treatment can significantly improve your chance of survival.