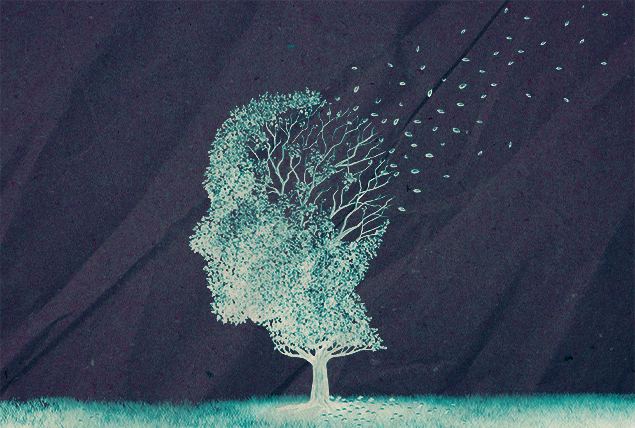
Living With Alzheimer's: How to Cope With Relational, Sexual Changes

Living with Alzheimer's disease can be crippling, especially because the condition and its demential effects inevitably worsen. The patient's behavior and personality might undergo unexpected changes.
This could be tough for patients, family members and caregivers. Sexual health can also be concerning because the disease can affect sex drive. It lessens libido in most cases but can also cause an increased interest in sex, an obsessive and excessive behavior known as hypersexuality. The cause of these behaviors is more about a lack of comfort, feeling pain, confusion and loneliness.
What are the potential changes you should be mentally prepared for and what can caregivers do to facilitate communication?
Coping with symptoms in early- to mid-stage Alzheimer's
Early- to mid-stage Alzheimer's patients may experience mild symptoms of memory loss and cognitive decline, such as challenges in making decisions and carrying out daily tasks, and changes in mood. Each individual may not have the same symptoms or experience them to the same degree as others.
Nicole Purcell, D.O., M.S., a neurologist based in Harrisburg, Pennsylvania, and the senior director of clinical practice at the Alzheimer's Association, shared her insights and some practical tips.
At the start of the Alzheimer's journey, patients can opt for medications that help to prevent the worsening of these symptoms, she explained.
"They can help reduce memory loss and confusion, and increase attention for a time in certain individuals," she added.
Purcell encouraged people suffering from Alzheimer's to consider participating in clinical trials examining potential new treatments.
"Participation in these trials is free and provides access to high-quality care throughout the duration of the trial," she noted. "Research shows that people living with the disease who are involved in clinical trials tend to do somewhat better than people in a similar stage of their disease who are not enrolled in clinical trials, regardless of whether the experimental treatment works, due to the high quality of care provided during clinical trials."
Purcell also advised Alzheimer's patients and their caregivers to pay close attention to lifestyle changes and choices to improve their quality of life.
"During this stage, individuals can reduce stress, which may exacerbate disease-related symptoms, by taking control of their health and wellness," she explained. "This can include adopting healthy lifestyle choices, making plans to address future financial, legal and care plans, and focusing time and energy doing the things that are most important and meaningful."
Preparing for behavioral changes
People suffering from Alzheimer's may face difficulty communicating or struggle to find the right words to verbalize their thoughts and feelings, which may lead to anxiety, agitation or aggression in some cases.
"It is important for caregivers and others to recognize that these behaviors are not intentional, they are disease-related," Purcell explained. "Dementia-related behaviors are a form of communication and often are triggered by relatively minor events. The person may be uncomfortable, confused, anxious or have some basic need, such as being hungry, thirsty or having to use the bathroom. Being unable to communicate their thoughts, feelings and needs can cause the person to act out in unexpected ways.
"When caregivers encounter dementia-related behaviors, the first step should be to try and understand what is triggering the behavior," she added. "What is the person trying to communicate? Is the person in pain, cold, hungry, sad or bored? Is the person bothered by something in their environment? Sometimes changing the environment or reassuring the person you are there for them can help minimize the behavior."
Here are five tips caregivers can use to adapt their communication to people suffering from Alzheimer's, based on Purcell's advice as well as other relevant resources:
1. Slow down, be clear and make eye contact
It's important to slow down as you speak, address the person by name and make eye contact with them.
“Use short, simple sentences," Purcell said. "Ask one question at a time, rather than overwhelming the person with a series of questions. Give the person time to process and respond before continuing the conversation."
Ask yes or no questions instead of open-ended ones.
2. Encourage conversations
Include the person in conversations and listen to their thoughts, feelings and needs. This makes them feel supported and heard.
Using humor can also lighten the mood.
3. Give clear step-by-step instructions for tasks
Long requests or instructions can be overwhelming. Go slow and give clear instructions step by step, ensuring the person understands what to do at every step.
You can also give visual cues and demonstrate how to complete the task. Written notes may also be helpful for them.
4. Be gentle, patient and reassuring
People suffering from Alzheimer's require patience and encouragement, as they can get anxious or frustrated with themselves as well as the person communicating with them.
Go slow and reassure them to ensure they feel safe.
"Being kind, gentle and relaxed can go a long way toward diffusing many dementia-related behaviors," Purcell said.
Try to avoid arguing as this could worsen dementia-related behaviors. If you don't agree with what the person says, let it go.
5. Encourage nonverbal communication (late-stage Alzheimer's)
When communicating with people suffering from late-stage Alzheimer's, if you don't understand what they are trying to convey, you can ask them to point or gesture.
You can guide the person by using gentle touch and the other four senses (sight, hearing, taste and smell) to communicate with them.
Most importantly, take into consideration the emotions that are expressed (instead of the words used), and treat the person with dignity and respect.
Coping with changes to sexual health and needs
A person diagnosed with Alzheimer's may experience changes in their sexual needs, drive and behavior. Their partner, especially if they are the primary caregiver, could also be stressed by the demands of caregiving, which in turn could affect their sexual desire toward their partner.
"It's common for either partner to lose sexual desire as dementia may cause changes in personality, roles or energy levels," Purcell explained.
People with Alzheimer's generally need to feel loved and cared for, but the kind of emotional and physical intimacy they share with their partner is likely to be different due to cognitive decline.
"If a decrease in sexual desire becomes problematic for either partner, consult with your doctor to determine if there is a medical cause for the change. Common reasons may include a physical illness not related to dementia, a hormonal imbalance, side effects of medication or depression," Purcell advised.
"Try not to take changes in sexual desire personally," she added. "It's normal to feel lonely and rejected, and it may help to talk to your partner or someone you trust about these feelings."
Here are two examples of how couples can maintain intimacy:
Use nonsexual physical touch as a substitute for sex
Couples can cuddle, hug, hold hands, massage or touch each other nonsexually to show affection for each other. This can help them relax and maintain emotional intimacy even if sexual desires have changed in one or both partners.
"Navigating changes in sexuality and the expression of physical or emotional closeness with your partner is deeply personal and there is no single approach that will work for every couple," Purcell said. "Do what feels best for you and try not to feel guilty if sex is no longer a priority. Find new ways to connect that are mutually satisfying."
Connect through other meaningful moments together
Couples can connect with each other through meaningful moments such as sharing a meal, watching a movie or taking a walk together.
Seeking intimacy outside the relationship
As Alzheimer's disease results in further cognitive decline in a person and they reach late-stage Alzheimer's, it can create further challenges in a couple's relationship.
Late-stage caregiving can prove intensive and challenging. Depending on the circumstance, moving the person with late-stage Alzheimer's to a professional care facility could be a more effective option for them to get the full extent of care they need.
Before the person reaches this stage, important subjects such as end-of-life care wishes should be discussed while they still have the capacity to do so.
These discussions can include how the caregiver spouse can still love and care for the partner with Alzheimer's while moving forward with their life, such as perhaps having another partner to fulfill their sexual and/or emotional needs.
Caregivers might struggle with loneliness as their relationship with their partner is no longer the same, especially if their partner can no longer recognize them. They might want to move on with their life and seek a new partner but struggle with guilt.
In such cases, caregivers can consider discussing the subject with a trusted professional therapist as they're making important decisions, Purcell advised.