How Celiac Disease Is Diagnosed—and the Consequences of Ignoring It
You've likely heard about celiac disease. You've also likely heard about gluten and how some people can't process it. But what the heck does it mean? Is celiac disease something you need to know more about?
It could be.
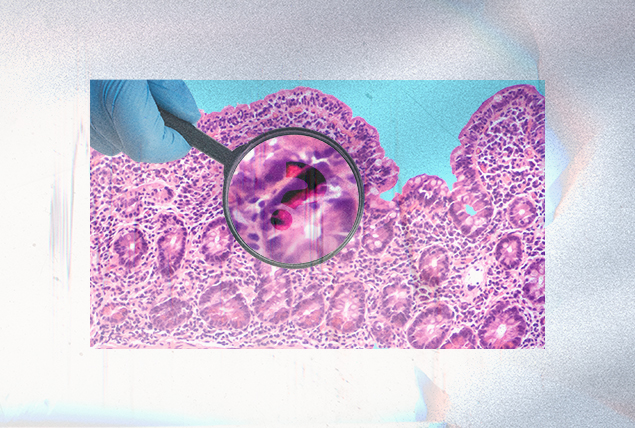
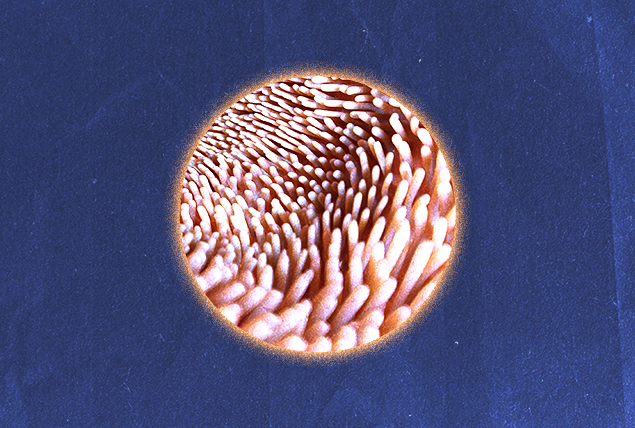
Celiac disease (CD) is a genetic autoimmune disease in which people are affected by negative reactions to gluten, a protein found in wheat, rye, barley and triticale. When a person with CD digests gluten, the body responds by launching an attack on itself. Over time, these attacks damage the small, fingerlike projections known as villi that line the small intestine. This is what's known as an immune reaction.
Unfortunately, not enough people—healthcare professionals included—know enough about the disease. That's why the average time span to arrive at a celiac diagnosis is six to 10 years.
Symptoms of celiac disease
"Symptoms may include diarrhea or constipation, weight loss, bloating, gas, abdominal pain, nausea and vomiting," said Blanca Garcia, a registered dietitian nutritionist in Los Angeles. "A combination of diarrhea and vomiting may cause dehydration. It's important to provide fluids for rehydration."
Celiac disease is well known for its varying and ambiguous manifestations across patients. This presents a unique challenge to nonverbal individuals like infants and adults with speech difficulties, according to Alice Bast, the CEO of Beyond Celiac in Ambler, Pennsylvania, and a celiac sufferer herself.
"Celiac disease may present itself in children with a sign or symptom that is visible, such as tooth enamel discoloration, canker sores or a celiac-specific rash called dermatitis herpetiformis," she said. "A child, verbal or nonverbal, may act out or become irritable from feeling ill, or they may have diarrhea, constipation or vomiting."
Dermatitis herpetiformis is a chronic, blistering rash that's extremely itchy and manifests in 10 percent of all individuals with CD. Small clusters of symmetrical papules, which resemble whiteheads but don't produce pus and vesicles (cysts), erupt on the elbows, knees, rear end, back, scalp and face.
While celiac disease is typically thought of as presenting with gastrointestinal symptoms, it's no surprise the disease impacts skin health. Skin is the body's largest organ.
Most frustratingly, the disease also may be asymptomatic despite the fact it is actively damaging the small intestine. So how does someone look for an invisible disease?
How celiac disease is diagnosed
"Celiac disease can be asymptomatic in many people, including children," said Aniruddh Setya, M.D., a pediatric gastroenterologist with Memorial Health Network in South Florida. "[It can] present with just mood changes in some and can present with severe gastrointestinal symptoms. Celiac disease has varied presentation and can only be diagnosed with the help of a physician, blood test and an endoscopy."
Obtaining this diagnosis begins simply.
"Celiac disease testing starts with a simple blood test, which looks for antibodies to gluten," Bast said. "If the blood test is positive, a patient will then receive an upper endoscopy with biopsies to confirm the diagnosis."
An endoscopy is a procedure in which the doctor, usually a gastroenterologist—an M.D. that specializes in gastrointestinal conditions—inserts a camera into the mouth, down the esophagus, into the stomach and then on to the small intestine to evaluate damage there. Patients are sedated during the procedure.
The rashes caused by celiac disease offer another route to obtaining a diagnosis.
"The skin manifestation of celiac disease may be diagnosed by a dermatologist with a skin biopsy," Bast said. "If positive, a gastroenterologist would do an endoscopy and biopsy to determine if the patient has celiac disease and make the final diagnosis."
When to seek help for celiac disease
Setya provided a caveat for testing: Even if you want to get better now, get a diagnosis before altering your diet.
"The blood tests and endoscopy need to be done while you are still consuming a gluten-rich diet," he explained. "These tests will be altered if you are already on a gluten-free diet and are often used to determine your compliance to a gluten-free diet on your annual follow-ups with your doctor."
OK, so what's the threshold for determining when to schedule an appointment?
"According to Mayo Clinic, you should call your doctor if you have pain that is so bad that you can't move without causing more pain or if you can't get comfortable," Bast said. "However, celiac disease has many potential symptoms other than just stomach aches, including anemia, neuropathy, brain fog, vomiting or stunted growth."
Many diagnoses are obtained because the person suffers from symptoms, but that's not the only reason to get tested. Celiac disease is a genetic condition, so your likelihood of being diagnosed with it is partly based on how closely related you are to someone who has already been diagnosed.
First-degree relatives—these include parents and full siblings—of someone with celiac disease have about a 1 in 13 chance of developing it, depending on relationship and geography. Extended family and half-siblings are second-degree relatives. If they're diagnosed with the disease, you have a 1 in 39 chance of also testing positive for it—even with no apparent symptoms.
This testing is essential. Your quality of life may not have been impacted yet, but CD can be doing damage to your small intestine.
Consequences of not treating celiac disease
Information and self-education ideally expedite the entire process, but there are dangers of not adapting your diet after you obtain a diagnosis.
"Constant exposure to gluten can make the disease progressively more aggressive," said Joseph Shami, M.D., a gastroenterologist with Gastroenterology Associates of New Jersey. "[Symptoms range] anywhere from general malaise to abdominal pain, headaches, rashes, joint pains, diarrhea, weight loss, anemia, confusion. There has been one published report of a fatal case. However, fatal diseases can develop from untreated celiac disease."
In the long term, untreated CD can foster malnutrition and lead to osteoporosis. There's also a connection between untreated celiac disease and certain types of cancer, such as a rare non-Hodgkin lymphoma called enteropathy-associated T-cell lymphoma (EATL) and adenocarcinoma of the small intestine.
Neurological consequences of untreated celiac disease include gluten ataxia and peripheral neuropathy. Ataxia can emerge as the disease damages the cerebellum, resulting in a loss of coordination. Peripheral neuropathy is the numbing and tingling of body parts.
These two conditions, numbness and clumsiness, can compound each other and could lead to dangerous falls. With osteoporosis in the mix, the consequences can be dire.
Celiac disease is a shape-shifting disease that is sometimes even invisible. Open and honest communication with your healthcare professional is essential in diagnosing the condition before it can cause damage to the small intestine and beyond.
If you don't have a doctor you see regularly, you should find one, especially if you're experiencing symptoms. Fortunately, telehealth makes it easy to connect with a doctor who can answer your questions and evaluate your situation. Many physicians offer video visits, which are a good way to see a doctor quickly. And if follow-up testing is required, you've established a relationship.
Giddy telehealth is an easy-to-use online portal that provides access to hundreds of healthcare professionals whose expertise covers the full scope of medical care. A lot of them accommodate same-day appointments, so no time is wasted.