
What Happens When Sexual Health Services Are Inadequate?
Sexual health is integral to people's overall health and well-being, according to the Centers for Disease Control and Prevention (CDC), with effects that extend far beyond the bedroom. Where sexual health services are lacking—including testing and treatment for sexually transmitted infections (STIs), reproductive care and sex education—the impact is felt by individuals, families, communities and the nation as a whole.
"Your sexual organs are one part of your body, and if you're not able to take good care of your sexual health, it will have other impacts on your health," said Rebekah Horowitz, M.P.H., a senior program analyst working on the HIV, STI and viral hepatitis program at the National Association of County and City Health Officials (NACCHO) in Washington, D.C. "Additionally, if you're not able to access healthcare and get birth control or make the decisions about your body—about when and why and where you want to have children—that also affects your physical health and mental health. Anytime that we are not giving people adequate information and access to resources, we are affecting their health. And that is public health."
"Where sexual health services are inadequate, there is a significant negative impact on overall public health and well-being," said Vincent Guilamo-Ramos, Ph.D., M.P.H., the dean of the Duke University School of Nursing in Durham, North Carolina, in an email interview.
Guilamo-Ramos added that sexual health services may be inadequate due to a lack of availability, accessibility or quality. These inadequacies can have a few primary effects. First, he noted that a lack of adequate and comprehensive sexual health services increases the incidence of adverse sexual and reproductive health outcomes associated with substantial population-level morbidity, including:
- STIs
- Cervical and other cancers
- HIV infection
- Unplanned pregnancies
Then there are broader social welfare implications.
"For example, teen pregnancies and parenthood increase the risk of not completing high school education for both teen mothers and their children down the line," Guilamo-Ramos said. "In addition, many sexual health issues, such as HIV infection, remain associated with substantial societal stigma—and criminalization in some states—which can have wide-reaching consequences for the well-being, life opportunities and long-term health outcomes of people living with HIV."
As Guilamo-Ramos and Horowitz noted, sexual health service inadequacies can produce broad and substantial consequences. In addition to challenges such as painful sex and erectile dysfunction (ED), potential ramifications include an increased risk of unplanned pregnancies and various chronic conditions, from pelvic inflammatory disease (PID) to cancer.
Whether planned or not, pregnancy and birthing can produce a variety of acute and lasting health effects, including eclampsia, postpartum hemorrhage, bladder dropping, stress incontinence, rectocele, parental stress and mood disorders, such as postpartum depression and anxiety. The risk of long-term health effects is higher with unintended pregnancies.
Exposure to STIs can make a person more vulnerable to subsequent health issues. According to the CDC, untreated syphilis can damage the nervous system, heart, eyes and other organs. It can also cause infertility and increase a person's likelihood of contracting HIV and other diseases. Hepatitis can lead to liver disease. Human papillomavirus (HPV) causes more than 9 in 10 cervical cancer cases. Hepatitis and HPV could be nearly eradicated with widespread vaccinations and testing, yet a recent study found late-stage cervical cancer is on the rise in the United States due, in part, to vaccine hesitancy and missed screenings.
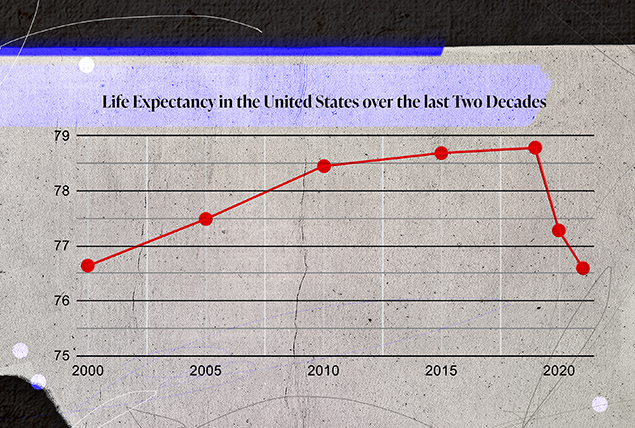
In the most significant decline in a two-year period since the 1920s, the average life expectancy in the U.S. dropped from 78.79 years in 2019 to just over 76 years in 2021, according to a recent CDC report.
Of course, the impact of COVID-19 was substantial, but it's far from the only factor affecting mortality. After COVID-19, the CDC implicates drug overdoses, heart and liver disease, accidental injury and suicide as the leading contributors. Some factors, though not all, are directly or indirectly related to sexual health.
"Life expectancy in the U.S. decreased meaningfully during the pandemic. What's important to realize, though, is that the excess mortality during the pandemic only in part stems directly from COVID-19 infections but is also associated with disruptions in care for other, primarily chronic, conditions," Guilamo-Ramos said.
These chronic conditions include breast, cervical, colorectal and prostate cancers. Cancer deaths have generally declined in the past several years, but the disease remains among the top causes of death in the United States. Cancer prognoses vary substantially from one patient to another, but outcomes tend to improve dramatically with early detection and intervention, services that may not be available or accessible where sexual health services are lacking.
Suicide, notable as one of the primary factors of lower life expectancy cited by the CDC, disproportionately affects marginalized populations, including members of the LGBTQIA+ community, especially transgender people. Data indicates 82 percent of trans people have considered suicide, and 40 percent have attempted to take their own lives. Trans youth are particularly at risk, which is something that comprehensive and inclusive sex ed and sexual health services could help mitigate.
Furthermore, a 2022 study that collated data from 1974 to 2016 found suicide rates were higher among people of reproductive age in states with abortion restrictions. This finding mirrors other research, including the 2018 Turnaway Study, which indicated people unable to access abortions may be more likely to have mental health conditions such as stress, anxiety and low self-esteem after unsuccessfully seeking termination, compared with women who received abortions.
Another report published by the Commonwealth Fund in December 2022 found states that have or are likely to pass abortion restrictions tend to fare worse in mental health outcomes. Researchers found states with complete, partial or planned bans or restrictions also had fewer maternity care providers, more maternity care "deserts," and higher rates of maternal mortality and infant death compared to the national average, especially among people of color. Additionally, these states had higher overall death rates for women of reproductive age and greater racial inequities in healthcare overall.
Young people who don't have access to inclusive, comprehensive sex education and sexual health services are more susceptible to various adverse outcomes, including STIs and unplanned pregnancies, according to Planned Parenthood and a 2022 study published in the Proceedings of the National Academy of Sciences (PNAS).
The burden is heavier still for LGBTQIA+ youth, who may face additional questions about their gender and sexuality and have fewer resources for education and support. LGBTQIA+ people, including youth, are also at higher risk of adverse health outcomes, the CDC reports. Many LGBTQIA+ youths have a limited number, if any, of trusted adults they can turn to for help, according to the Human Rights Council (HRC) and a study published in the journal Health Education Research. Medically accurate, inclusive and comprehensive sex ed could help to fill that void, according to the HRC, CDC and SIECUS, the Sexual Information and Education Council of the United States. If sex ed is inadequate, young people may turn to the internet or peers, sources that may prove insufficient or even detrimental, according to the HRC and Planned Parenthood.
Additionally, a study published in 2021 in the Journal of Adolescent Health found medically accurate and inclusive sex education improved mental health outcomes and reduced school-based victimization for LGBTQIA+ students.
"Obviously, if you're getting no education or incorrect education, it means that you are less prepared to take protective behaviors and do things that will put you in the best possible health," Horowitz explained. "If you've never learned about STIs or never learned about condoms or never learned about birth control, you are not going to be avoiding those things or using those things. You're not being given all the information that you need to make the informed decision about what's right for your sexual health and how you want to be engaging in sexual health or sexual practices safely."
Young adults aren't the only group impacted by inadequate sexual health services. Babies born from unintended pregnancies tend to have lower birth weights and shorter duration of breastfeeding. This can result in lasting consequences, such as a greater likelihood of diabetes, leukemia and sudden infant death syndrome (SIDS).
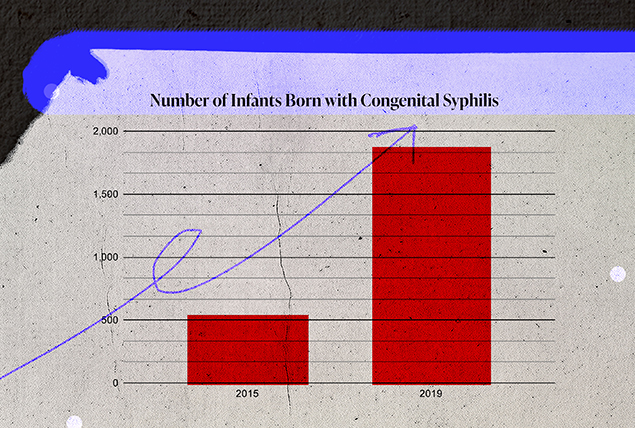
Inadequate reproductive healthcare services can also increase the risk of fetal illnesses, including STIs such as HIV, gonorrhea, chlamydia, hepatitis B, congenital syphilis and genital herpes. In 2019, the CDC reported 1,870 infants were born with congenital syphilis, a 291 percent increase from 2015.
According to the U.S. Department of Health and Human Services Office on Women's Health, potential complications caused by fetal STIs include:
- Acute hepatitis
- Blindness or deafness
- Brain damage
- Chronic liver disease
- Infections of the blood or eyes
- Low birth weight
- Meningitis
- Mobility challenges
- Pneumonia
- Stillbirth
Akin to the substantial disparities in maternal morbidity and mortality by race and ethnicity, there are equally significant disparities for infants.
"We have ongoing inequities in infant death rates by race and ethnicity, with particularly high rates for Black infants. Some of this, we know, is related to higher rates of preterm delivery in Black families," said Arden Handler, Dr.P.H., a professor and the director at the Center of Excellence in Maternal and Child Health at the University of Illinois Chicago School of Public Health. "But we also know that there's a large disparity in infant death rates in the postneonatal period."
Many of the issues in the postneonatal period, she noted, relate to inadequate food and lack of housing, and poverty in general. Limited access to healthcare services and parents' inability to take time off from work also substantially affect infants during this vulnerable period.
A parent's inability to access desired contraception and abortion services can impact children, too. Research shows most people who seek abortions already have children and many cite financial difficulties as one reason for seeking pregnancy termination.
"Individuals who want abortions often have two or three kids and they can't afford another child," Handler explained.
Handler added that unintended pregnancies and births can exacerbate existing stress and poverty, affecting the entire household and increasing the likelihood of family stressors and adverse outcomes that can affect birthing parents and children for life.
"We take a life-course perspective. We know that what is happening to a person during pregnancy—those experiences in utero—affect fetal well-being, and then infant and child well-being," she said. "And as the child grows up, some of the exposures from early life, either in utero and early life stressors, end up manifesting in future health status. Cardiovascular health status, diabetes and hypertension can also affect future reproduction."
"Inadequate sexual health services contribute to persistent health inequities in the U.S. Health inequities are associated with notable human and financial costs, both of which are unsustainable," Guilamo-Ramos said. "The human costs of sexual health inequities, such as unplanned pregnancies and STIs, include excess morbidity, unfulfilled human potential, increase [in] unpaid caregiver reliance, etcetera. In addition, negative sexual health outcomes are associated with billions of dollars in annual expenditures for health and social programming. Moreover, a recent Deloitte study estimated that the annual cost of all health inequities in the U.S. may reach $1 trillion by [2040] if the underlying causes remain unaddressed."
Unintended pregnancies may be the most dramatic example of the economic impact of insufficient sexual health services, according to Kristen Mark, Ph.D., M.P.H., a professor and the Joycelyn Elders chair in sexual health education at the Institute for Sexual and Gender Health at the University of Minnesota Medical School in Minneapolis.
"If we could eliminate unintended pregnancy, we would nearly eliminate the poverty cycle," she added.
Mark explained unintended pregnancies—which account for nearly half of all pregnancies in the United States—perpetuate the poverty cycle, making it perhaps the most impactful and important argument for comprehensive and inclusive sex education. She added that the lack of support services for parents exacerbates the financial burden of pregnancy and birth. Childcare is so expensive and public services so insufficient that many people living in poverty cannot work because their pay doesn't outweigh the cost of care.
'A recent Deloitte study estimated that the annual cost of all health inequities in the U.S. may reach $1 trillion by [2040] if the underlying causes remain unaddressed.'
Rachel Fey is the vice president of policy and strategic partnerships at Power to Decide, a Washington, D.C.-based national nonpartisan, nonprofit organization dedicated to reproductive well-being for all. She referred to the Turnaway Study, which demonstrated dramatic consequences for people unable to receive desired abortions.
The study compared people of similar limited economic means, including some who were able to access a desired abortion and some who weren't. The researchers found those who couldn't access a wanted abortion were significantly more likely to remain in poverty and stay in abusive relationships—among other adverse outcomes—years after they first sought an abortion. Fey noted this is attributable to many factors, including economics and access, particularly in the post-Roe era.
"In this world in which so many states have banned abortion care, right now it is a privilege to be able to travel out of state, pay for that care out-of-pocket and access the care you need," she explained. "The Turnaway Study really underlines what that means, particularly for people who are struggling to make ends meet. And it's devastating."
The cost of managing health conditions and paying for healthcare affects people who don't become pregnant, too. Research demonstrates people with chronic conditions, including sexual health ailments and related disorders, are more likely to experience income insecurity or poverty compared to generally healthy people. Moreover, the disproportionately high prevalence of chronic conditions within marginalized communities can perpetuate inequality and prevent societies from flourishing.
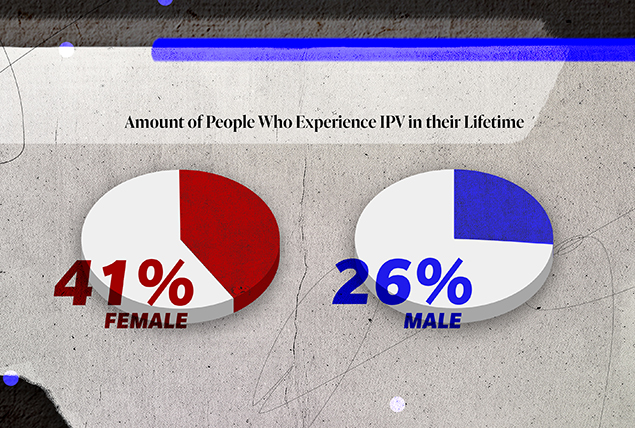
"Intimate partner violence [IPV], in general, remains far too prevalent in the U.S. Both women with and without access to abortion care reported experiencing physical and psychological abuse by their partners at unacceptably high rates," Guilamo-Ramos said. "Additionally, while discussions surrounding IPV tend to focus on women, over a quarter of all men have experienced IPV from a female or male partner. Increased efforts to reduce intimate partner violence deserve attention as a crucial component of improving comprehensive sexual health promotion in the U.S."
The promotion of sexual health includes how to prevent and address sexual coercion and violence. As such, sexual and reproductive health services should include screening for coercion and violence in relationships. They should also provide adequate support and resources where needed, he added.
"Where these elements of comprehensive sexual health services are lacking, opportunities for reducing intimate partner violence are missed," Guilamo-Ramos said.
Intimate partner violence and emotional and psychological abuse transcend demographics, but some groups, including pregnant and postpartum people, are more susceptible than others. According to the National Resource Center on Domestic Violence, nearly 20 percent of pregnant women experience violence, with teens and those with unintended pregnancies most affected.
According to the New England Journal of Medicine, homicide is the leading cause of pregnancy-associated death in the U.S. Pregnant and postpartum people are more than twice as likely to die from homicide than from hemorrhage or hypertensive disorders.
Guilamo-Ramos noted that a lack of accessible, quality sexual health services—including pre- and postnatal care—reduces crucial intervention opportunities. At the same time, inadequate contraception and abortion services elevate people's risk of exposure. This was demonstrated by the Turnaway Study, which found people who could not receive desired abortions were more likely to be victims of physical violence at the hands of an intimate partner than people who received the abortions they sought.
Research demonstrates people with chronic conditions, including sexual health ailments and related disorders, are more likely to experience income insecurity or poverty compared to generally healthy people.
For many, the abuse persisted for years after giving birth. People forced to carry a pregnancy to term were more likely to stay with abusive partners, bound by financial dependence, legal obligations and the logistical challenges of child-rearing.
People with STIs, especially HIV, are also more likely to experience abuse.
Neither domestic violence nor HIV causes the other, but for multiple reasons, many people grappling with one must navigate both, according to Courtney K. Cross in her article "The Dangers of Disclosure: How HIV Laws Harm Domestic Violence Survivors," published in 2020 in the Washington Law Review. Cross is an assistant professor of clinical legal instruction and the director of the Domestic Violence Law Clinic at the University of Alabama School of Law.
As she explained, just as abusive relationship dynamics may increase a person's risk of contracting HIV—for example, as a result of coerced sex or rape—a person's HIV status can be a vulnerability for an abusive partner to exploit.
"An initial diagnosis or notification of one's status can open the door to a host of physical and emotional forms of retaliation," she wrote.
In some cases, this retaliation includes falsifying claims that an individual failed to disclose their STI status. The CDC reports that 35 states have laws criminalizing STI exposure, primarily focusing on HIV. While such legislation was purportedly enacted to protect the public and prevent the spread of STIs, research indicates it does more harm than good.
A study published by the CDC showed no evidence that such laws reduce virus transmission. Other research suggested the laws may increase transmission rates because they perpetuate fear and stigma, resulting in a diminished likelihood of people being tested.
In addition, Guilamo-Ramos noted that such laws aren't rooted in science, as effective HIV treatment can suppress viral loads to undetectable levels and render them untransmittable.
"The U=U [undetectable equals untransmittable] principle negates any scientific basis for HIV criminalization," he said. "In contrast, HIV criminalization laws amplify the stigma and discrimination that remains associated with HIV and keeps people at risk of and living with HIV from seeking prevention, testing and treatment services. HIV stigma remains a key barrier for the existing and effective HIV prevention and treatment tools to reach all people who can benefit from them."
The next installment of the State of Sexual Health series will build on the concept of inadequate services and examine the sexual health challenges that face the U.S. as a society. These include the STI/STD surge, access to care for everyone, the state of sex education, the COVID-19 pandemic and the shifting landscape around reproductive rights.









