Various cancers can affect the female reproductive system, and the ones that get the most attention are cervical cancer and ovarian cancer. However, much rarer is vulvar cancer, which occurs on the outer surface of the female genitalia and is most often diagnosed in older women.
The Facts About Vulvar Cancer
Find out how vulvar cancer affects your sexual health.
Is vulvar cancer common?
The American Cancer Society estimated that about 6,330 vulvar cancer cases were diagnosed in 2022 and about 1,560 women were likely to die of this cancer during the year.
It's rare to find vulvar cancer in women younger than 50 who have not experienced menopause. Most women affected are older than 65.
Vaginal vs. vulvar cancer
The terminology for the vulva and vagina is often confused, but they are two different parts of the female reproductive system. The vulva is the outside of the female genitals, including the labia majora, labia minora and clitoris. The vagina is the internal hollow tube that connects the uterus to the outside of the body (sometimes called the birth canal).
Vaginal cancer is extremely rare—around 3,000 cases are diagnosed in the United States every year—and occurs on the inside of the vagina. The human papillomavirus (HPV) usually causes vaginal cancer, which is very slow to develop and grow.
Vulvar cancer most often occurs in the labia (labia minora and labia majora) but can also affect the clitoris. It can also affect the Bartholin's glands, which are located on each side of the vaginal opening and whose function is to secrete fluid that helps lubricate the vagina.
Symptoms of vulvar cancer
Symptoms of vulvar cancer can include:
- Bleeding from the vulva
- Blood-stained vaginal discharge between periods
- Burning pain when passing urine
- Lumps on the vulva that may be wart-like
- Open sores or rashes in the vulva
- Pelvic pain, especially when passing urine or having sex
- Red, white or dark raised and thickened patches of skin
- The vulva is painful, sore or tender
- A vulvar mole that changes shape or color
- Vulvar itching that doesn't go away
It should be noted that these symptoms don't always mean you have vulvar cancer. They are also the symptoms of many other problems. However, if you experience any of them, you should see your healthcare provider right away to find and treat the cause of the problem.
Causes and risk factors
The exact cause of vulvar cancer remains unknown, but research has identified several risk factors:
- Having a condition, such as HIV, that weakens your immune system
- Having a vulvar skin condition known as lichen sclerosus
- Infection with certain types of HPV
- Older age
- Previous vulvar or vaginal precancer
- Smoking
- The presence in the vulva of abnormal cells, which are at risk of turning cancerous. These are called vulvar intraepithelial neoplasia (VIN).
Diagnosis and testing
If you notice any unusual symptoms in your vagina or on your vulva, have abnormal changes in your vaginal discharge or periods or bleeding in between your periods or after menopause, the first step is to see your healthcare provider. They can explore your medical history and family history, gain an understanding of your symptoms, and possibly conduct a physical examination of your vulva, vagina and cervix.
If your doctor thinks it's necessary, they will refer you to an OB-GYN (obstetrician-gynecologist) who specializes in treating conditions of the female reproductive system.
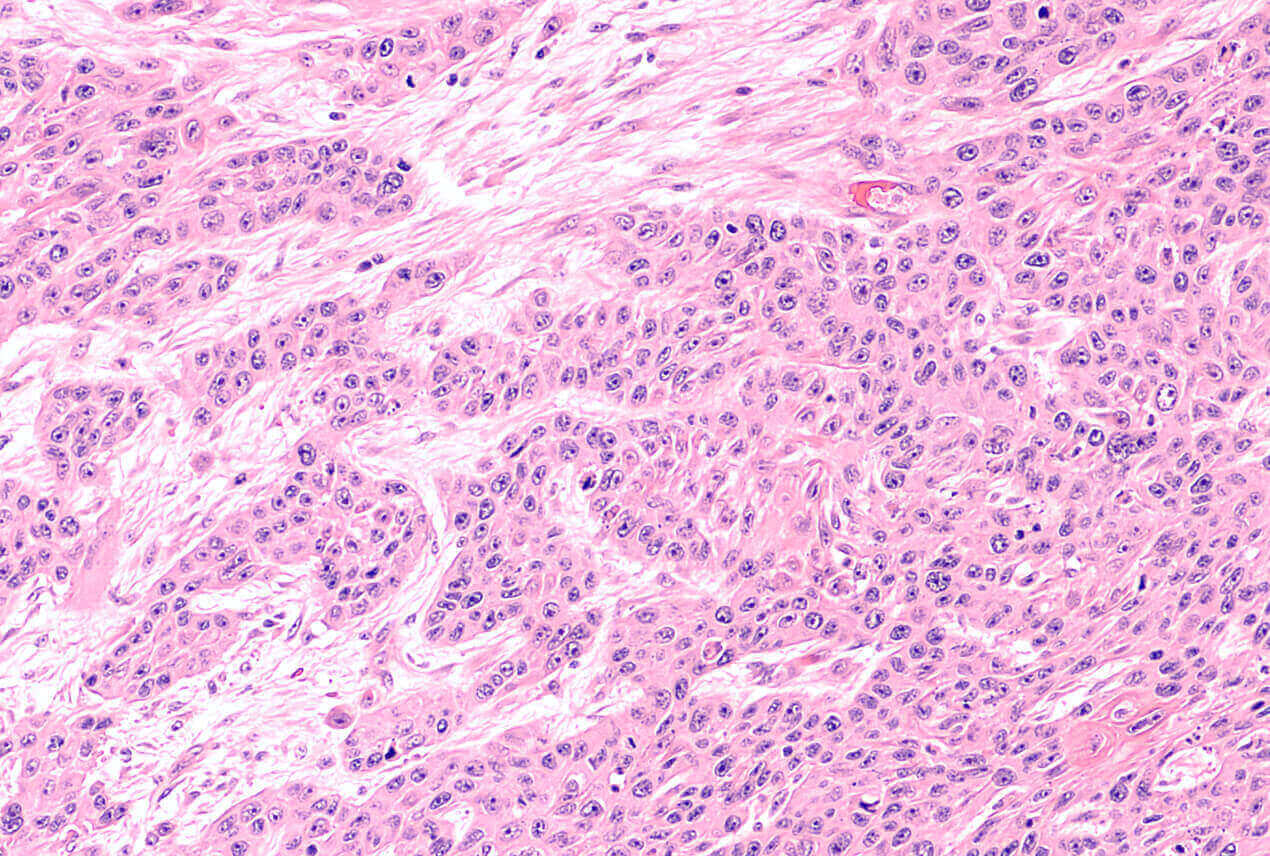
The next step toward a diagnosis of vulvar cancer may involve a biopsy. A clinician removes a small sample of tissue from the vulva so they can examine it under a microscope to see if the cells are cancerous.
You might need further tests to see if vulvar cancer has spread. They might include:
- Colposcopy. Checks for abnormal cells in the vagina.
- CT or MRI scan. Checks for cancer in other body organs.
- Cystoscopy. Examines the bladder.
- Lymph node biopsy. Checks whether cancer has spread to your lymphatic system.
- Pelvic examination under general anesthetic. Thoroughly looks at the internal reproductive organs.
- Proctoscopy. Looks at the inside of the rectum.
- X-ray. Checks if cancer has spread to your lungs.
Your OB-GYN can determine which tests you need, depending on your individual symptoms. Blood tests can also help doctors understand how well your body systems and organs are working.
Prevention
There isn't a screening test for vulvar cancers in women who present no signs or symptoms. However, there are ways that you can help reduce your risk, such as:
- Regular PAP smears. Although the PAP smear does not screen for vulvar cancer, it can detect HPV and vulvar intraepithelial neoplasia (VIN), either of which can put you at a higher risk of developing vulvar cancer.
- HPV vaccination
- Paying attention to your body and knowing what is normal for you
- Practicing safe sex to help avoid HPV infection
- See your healthcare provider if you notice any changes in your reproductive organs, periods or vaginal discharge that are not normal for you.
- Stopping smoking
Don't delay in seeing your doctor if you notice any body changes that aren't what you'd expect for your body. Vulvar cancer is more easily treated when discovered early.
Treatments for vulvar cancer
The type of treatment you need depends on the type and stage of vulvar cancer you have. Precancerous cells (VIN) can be treated with topical treatments such as fluorouracil (5FU), a type of topical chemotherapy. Another topical therapy is imiquimod, which boosts the body's immune response to abnormal cells.
Topical treatments are used only for VIN and not invasive vulvar cancer.
The three main treatment types for vulvar cancer are:
- Chemotherapy can be given intravenously, topically or orally. It might be combined with surgery and/or radiation therapy.
- Radiation therapy uses high-energy rays to kill cancer cells. It is sometimes combined with chemotherapy, which is called chemoradiation.
- Surgery options might include laser treatment, excision surgery, a vulvectomy, vulvar reconstruction or pelvic exenteration.
As with all types of cancer, treatments can be complex and are individualized for the patient and their cancer. Your cancer care team can talk you through your treatment options at every stage.
Don't forget that living with cancer can hugely impact your emotions. Reach out to your doctor for emotional support and advice on support groups if you are struggling with your feelings, depression or anxiety.
When to see a gynecologist
The best way to notice if you have any changes in your reproductive health is to get to know your body and menstrual cycle. Make sure you see a gynecologist (or speak to your family doctor to refer you) if you:
- Have bleeding in between periods or after menopause
- Have persistent itching, pain or swelling of the vulva
- Have persistent pelvic pain
- Notice any changes in the normal appearance of your vulva
- Notice your vaginal discharge is bloody, smelly or abnormal in color
FAQs
What does vulvar cancer look like?
In many cases, you may not have any visible symptoms of vulvar cancer. However, you may notice your vulva looks different from normal, such as having:
- An area of skin that looks different. It might be lighter or darker than the normal skin around it or look pink or red.
- New bumps or lumps
- Open sores on the vulva
- Thickening of the skin of the vulva
- Wart-like lumps or rough-feeling patches of skin on the vulva
How does a woman get vulvar cancer?
The exact cause of vulvar cancer is unknown, but you are more at risk if you have certain types of HPV, vulvar intraepithelial neoplasia or a skin condition called vulva skin condition, also known as lichen sclerosus. It usually affects women older than 65 after menopause.
How dangerous is vulvar cancer?
Vulvar cancer is rare, which means it is harder to study. Despite this fact, effective treatments are progressing all the time, thanks to ongoing research.
The five-year survival rate for people with vulvar cancer is 71 percent and increases to 87 percent for vulvar cancer that has not spread beyond the vulva. Remember, survival rates are just estimates based on the general population and depend on many factors. Your doctor is the best person to talk to about your specific cancer, treatment options and survival rates.












