"Raising awareness" is such a tricky phrase.
It's a nice idea. Loads of well-meaning people have the best intentions when trying to raise awareness for this issue or that issue by signing online petitions, clicking the "like" button or retweeting something.
But let's be real: The vast majority of the time, being aware of issues facing us isn't what stands in our way. We know what the problems are. The question is, what are we going to do about them?
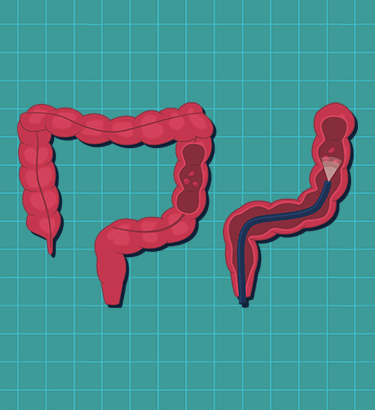
Colorectal Cancer Awareness Month in March gives everyone an opportunity to answer that question. Raising awareness of the third most common type of cancer for men and women in the United States can save lives—not tomorrow, not someday, not theoretically, but today, for you or someone you love.
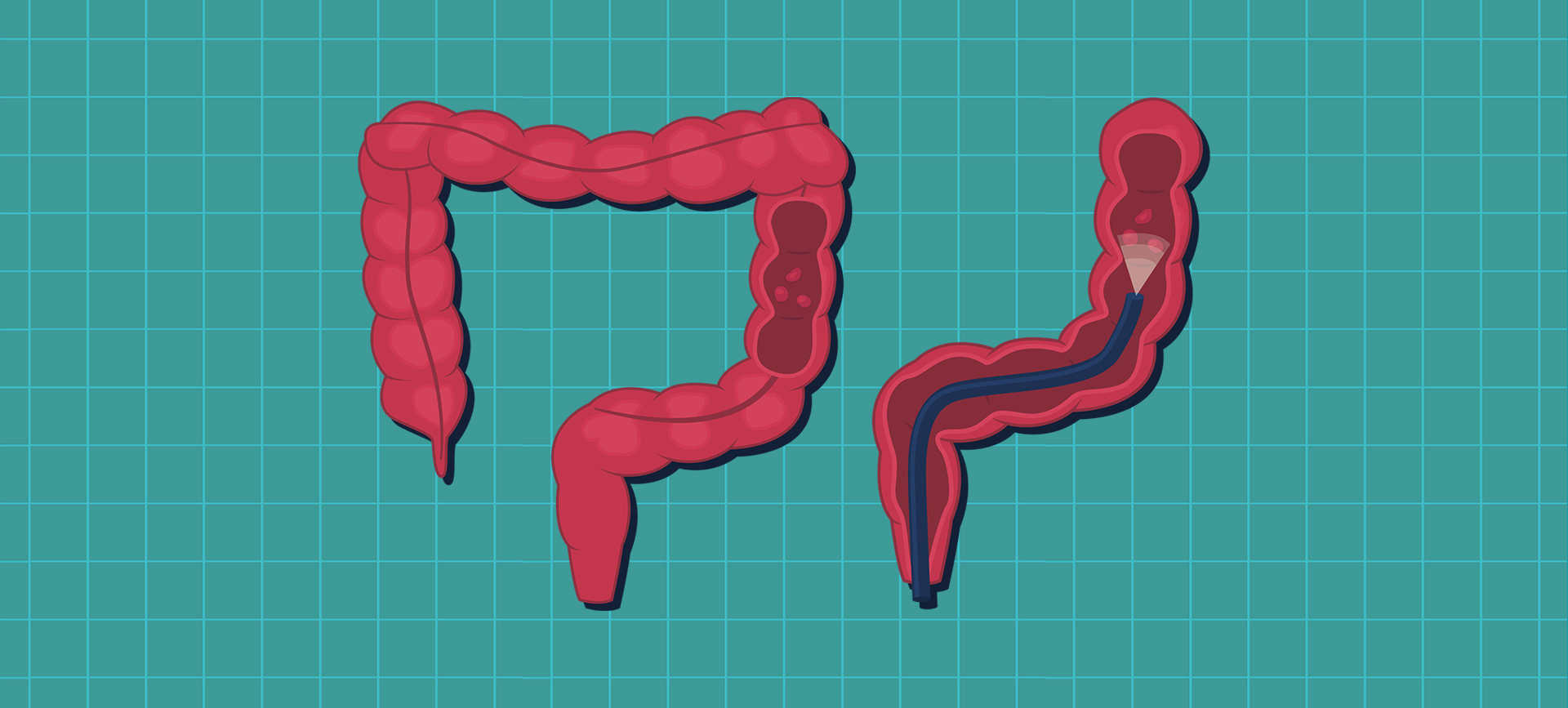
That's not hyperbole or exaggeration. Certain types of screening for colorectal cancer can remove the threat of it in real-time.
"The nice thing about colorectal cancer—well, there's nothing 'nice' about cancer—but colorectal cancer is one that you can actually screen for and prevent to a large degree, which is not something that's true of all cancers," said Shahrad Hakimian, M.D., a gastroenterologist with UCLA Health in Los Angeles. "We can basically prevent cancer from happening or catch it at a much earlier stage where it's more easily treatable and even curable."
Here's what you need to know about colorectal cancer screening, symptoms and diagnosis.