The hormonal birth control pill prevents pregnancy by preventing ovulation (the release of an egg) and by thickening cervical mucus, which makes it difficult for sperm to make contact with an egg if ovulation does occur.
Those tiny pills contain either progestin or a combination of progestin and estrogen. The bleeding you experience during the week of placebo pills is what doctors call "withdrawal bleeding." Your uterus sheds its lining because you've stopped taking the hormones.
"You're only seeing a reflection of what those hormones [in birth control] are doing to your body," as opposed to a natural cycle, explained Asima Ahmad, M.D., M.P.H., a board-certified reproductive endocrinologist and OB-GYN, and chief medical officer at Carrot Fertility.
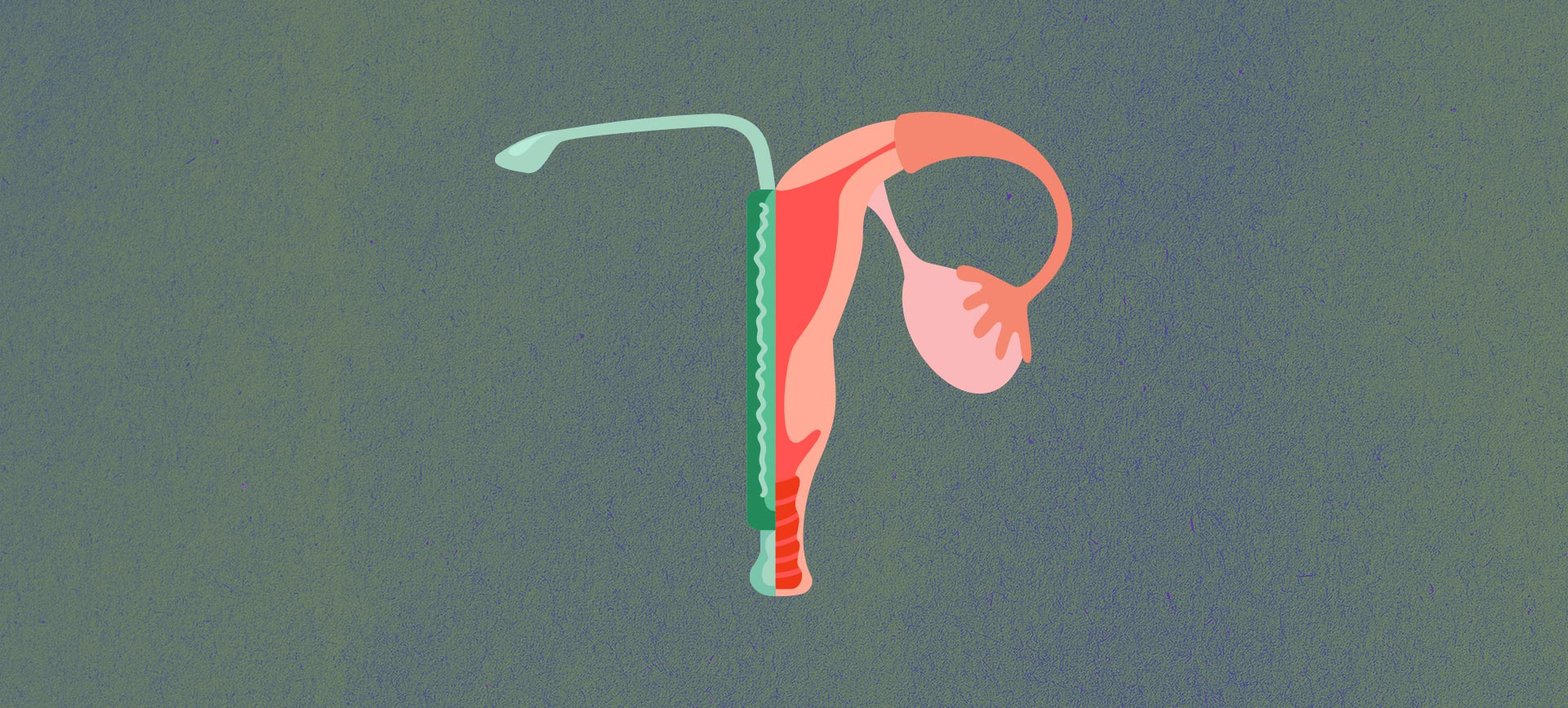
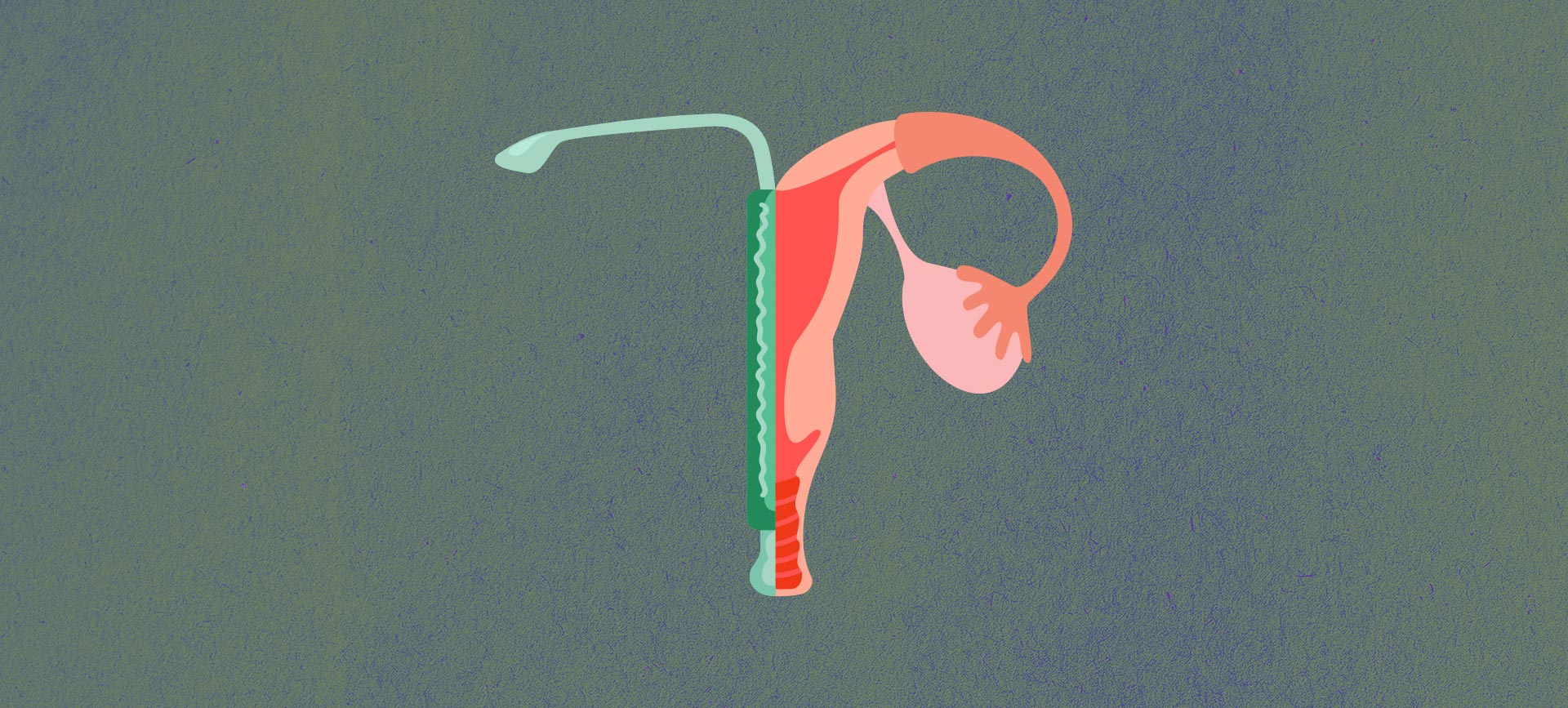
With hormonal IUDs, the hormones are released inside your uterus, where the IUD is placed, and most of the effect of IUDs is local. With a nonhormonal IUD (Paragard is the only brand available in the United States), it's the copper wrapped around the small piece of plastic that prevents pregnancy. Copper ions are directly toxic to sperm, likely causing an inflammatory response in the tissue of the uterus, which interrupts sperm's ability to swim, preventing them from reaching an egg (although some researchers disagree with the notion of inflammation).
With a nonhormonal IUD, ovulation continues to occur naturally. But for some women, the copper IUD does cause an increase in uterine bleeding and cramps. For most, these side effects fade. But for some, heavier periods can persist. My doctor told me I likely would have noticed my cycle getting shorter sooner had I not been experiencing a heavier period caused by my IUD.
Overall, research has shown the ways in which hormonal and nonhormonal birth control prevent us from getting pregnant have no lasting impact on our hormones or our fertility. A three-year study of oral contraceptives with more than 3,000 participants found that although there can be a delay in fertility after discontinuing use, there is no long-term effect on women's ability to conceive.