Certain Chronic Conditions That Cause ED Hit Veterans Harder

U.S. military veterans are at a higher risk of erectile dysfunction (ED)—the inability to get or maintain an erection satisfactory for sexual intercourse—than the general population.
That is the conclusion of several studies in recent years involving erectile dysfunction and veterans.
The numbers vary from study to study, ranging from a slightly higher risk to significantly higher. No matter the percentage, however, veterans—especially those younger than 40—typically experience ED more frequently because they are at a greater risk of experiencing so many of the chronic conditions that cause ED or contribute to it.
Some conditions are directly service-connected, while others are more indirect.
Timothy "T.J." Tausch, M.D., a urologist in Mansfield, Ohio and is affiliated with Avita Ontario Hospital, said there are two main categories defining veterans and sexual health:
- Those who have sustained combat injuries
- Those with the routine issues that come with aging
The risk factors for erectile dysfunction in veterans
Combat veterans may have sustained some type of physical trauma, such as an improvised explosive device (IED) attack or a crush injury. Some experience penetrating trauma and burns to the genitals. Spinal cord injuries are not uncommon.
And then there's the psychological impact, which includes post-traumatic stress disorder (PTSD), depression, generalized anxiety disorder and difficulties transitioning back to civilian life.
"I've had a bunch of patients with psychiatric issues that had erection problems," said Tausch, who spent 15 years on active duty in the Army. He also worked at Walter Reed National Medical Center, where he was the director of trauma, reconstructive and prosthetic urology.
"Anecdotally, PTSD just jumps right to the forefront of my mind. Depression, substance abuse—all those things that go along with the mental health aspect of veteran care—do contribute to sexual health and functional issues with that," he said.
Environmental factors may play a role as well. For example, veterans who were exposed to the herbicide Agent Orange during the Vietnam War are at a greater risk of developing prostate cancer, and surgery for the disease is linked to ED.
ED also becomes more common as men age, and the veteran population tends to be older, with an average age of 65, according to the U.S. Census Bureau.
Tausch believes one of the reasons veterans report ED at a greater rate than the general population is because they typically have better access to healthcare and may talk about it more.
"They might be able to seek help or have routine primary care appointments when they bring up these issues more frequently than the general population, which is a good thing and a success story for the VA and for the retirees with Tricare," Tausch said, referring to the U.S. Department of Veterans Affairs, which provides lifelong healthcare to eligible veterans. Tricare is a healthcare program that serves more than 9 million active-duty service members and retirees.
By the numbers
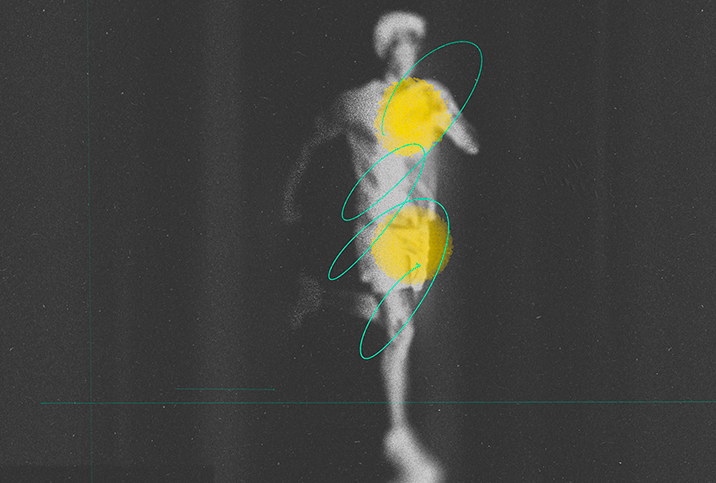
Some of the most common risk factors for ED include diabetes, hypertension, obesity and tobacco use.
The rate of diabetes among veterans is more than double that of the general population. One in 4 VA patients have diabetes, compared to 1 in 10 nonveterans, according to research in the journal Federal Practitioner.
Hypertension, or high blood pressure, is the most common chronic condition among veterans. It affects more than 37 percent of veterans, according to the VA. A study that analyzed nearly 40,000 service members found exposure to combat increases the risk of hypertension, and combat injuries exacerbate this risk.
Researchers believe this increased risk is due, in part, to changes in inflammatory responses and psychological stress.
Of the 6 million veterans who receive care from the VA each year, nearly 80 percent are overweight or obese. Studies show veterans not only have significantly higher levels of obesity but also more associated comorbidities when compared with nonveterans. These comorbidities include:
- Coronary heart disease
- Chronic obstructive pulmonary disease (COPD)
- Depressive disorders
- Diabetes
All of these are risk factors for ED.
While it's not apparent whether obesity directly causes ED or is merely tied to the associated risk factors, it's clear that it is a contributing factor.
Veterans also use tobacco products at much higher rates than most nonveterans, according to the Centers for Disease Control and Prevention (CDC). About 3 in 10 veterans used some form of tobacco product between 2010 and 2015.
"Smoking is a big risk factor," said Carolyn Salter, M.D., a urologist at Madigan Army Medical Center in Tacoma, Washington. "Smoking is incredibly bad for erections, just because it's bad for all your blood vessels. But the blood vessels to your penis are incredibly small, so any amount of plaque buildup can lead to erectile dysfunction."
Many men who stop smoking, eat a healthier diet and become more physically active may actually be able to reverse ED to an extent, she said, which could lead to an improved sex life.
"You could potentially avoid a medication if you change your lifestyle habits to a healthier regimen," Salter said. "That should be the first line for anyone."
In some cases, it's not the chronic condition but the medication being used to treat it that leads to ED. For example, many veterans experience chronic pain that may require them to take prescription narcotics and opioids. These pain medications may lower testosterone levels with prolonged use, and low testosterone might impact erectile and sexual function.
"When someone is constantly on an opiate, your hormone-mediated neurological response system is a little slowed and delayed, similar to like when men drink alcohol," said Helen Bernie, D.O., a urologist and the director of sexual and reproductive medicine at Indiana University Health. "They can reach a point where it's difficult or challenging to achieve an erection."
The effects of trauma and stress
Post-traumatic stress syndrome (PTSD) is perhaps the chronic condition most associated with veterans, particularly those who saw combat. Common symptoms of PTSD include reexperiencing combat or significant trauma during their service through intrusive recollections. These occurrences can come in the form of nightmares and flashbacks.
Veterans with PTSD may avoid places, people and activities that remind them of the trauma they experienced.
Of male combat veterans undergoing treatment for PTSD, 85 percent reported symptoms of ED, according to a 2002 study. By comparison, only 22 percent of men in the control group of the study experienced ED.
A 2021 cohort study, which included data from more than 1,000 patients, found men with PTSD had a higher risk of developing ED than men in a non-PTSD group.
"PTSD has the potential to negatively impact sexual functioning across multiple areas: desire, arousal, orgasm and fulfillment," said Louis Pagano, Ph.D., a clinical psychologist in St. Cloud, Minnesota, who has been treating veterans with PTSD since 2014.
It's believed that PTSD impacts erections because the disorder and sexual activity both come with physiological changes, and the body can only do so much at once, Pagano explained.
He said the first-line treatment options for PTSD are prolonged exposure and cognitive processing therapy (CPT). Prolonged exposure is a type of cognitive behavioral therapy (CBT) that helps veterans approach trauma-related thoughts, feelings and situations in a safe and gradual manner. This intervention strategy helps veterans confront their fears.
Cognitive processing therapy is a specific type of CBT that has been shown to be helpful in improving symptoms of PTSD.
Post-traumatic stress syndrome also frequently leads to sleep disturbances. Research shows that sleep deprivation and sleep disorders, such as sleep apnea, reduce a man's testosterone levels.
"That obviously would contribute to erectile dysfunction as well as lack of [sexual] desire," Tausch said.
Seeking treatment
It's important for veterans to talk to their primary care providers about any sexual dysfunction so they know about the resources available to them, Salter said. She finds many veterans are embarrassed to talk about their ED.
"If you have high blood pressure, that's something you might talk to your friend or your family about," she said. "But I think with the sexual dysfunction, a lot of people don't really speak to their colleagues about it."
Too many patients don't realize there are military doctors who deal with such issues, she added.
"Or they don't realize that maybe we cover these treatments," Salter continued. "Or they have no concept of the fact that we have surgical options for them as well."
Tausch echoed Salter, saying it's important for veterans to start with their primary care doctor, be it at the VA or in the community.
"Don't take no for an answer," Tausch said. "Just keep asking until someone gets you to where you want to be. And whether that's a referral to a urologist or a simple prescription for sildenafil, that can be all done. I tell my patients that as long as you still have a penis, we're going to have an option for you, most likely."
When medications don't do the trick, or you simply don't want to take more of them, a wearable device can help. Eddie® is an FDA-registered Class II medical device designed to treat erectile dysfunction and improve male sexual performance. It was specially engineered to treat ED without the discomfort of other wearables or the side effects of medication. The subtle size and fast-acting results of Eddie allow men to treat their ED with more control.
ED is a quality-of-life issue, and Tausch doesn't want to see veterans suffer in silence.
"People like me are all over the place, ready to help you out," he said.